Abstract
Review Article
Indoor air pollution and behavioral factors affecting to COVID-19 transition
Mojtaba Ehsanifar*, Mehravar Rafati and Zeinab Yavari
Published: 26 March, 2022 | Volume 3 - Issue 1 | Pages: 016-020
Environmental and behavioral factors are very important for exposure to airborne SARS-CoV-2. Indoor environments are related to infection events, including super-spreader events and outbreaks. Indoor, poorly ventilated, and crowded areas, such as restaurants, cinemas, and bars can be effective in the accumulation of aerosols full of viruses, especially if people are in conversations and stay there for a long time period. At longer distances (more than 1.5 meters), small aerosols that can stay in the air for a longer period of time are dominant. The super-spreader events in which people have been infected at a distance away show that this remote transmission occurs. The exposure risk to longer intervals is likely to be more in domestic environments and indoor spaces that lack sufficient ventilation. Layer interventions are of fundamental importance. Therefore, it is important to take preventive measures as much as possible and follow them as carefully as possible, because no intervention alone will be effective in eliminating the risk. These include spacing, lining, hand hygiene, filtration, and ventilation.
Read Full Article HTML DOI: 10.29328/journal.jcmhs.1001015 Cite this Article Read Full Article PDF
Keywords:
Indoor environment; COVID-19 transition; Airborne SARS-CoV-2; Behavioral factors; Indoor Air pollution
References
- Dong Y, Mo X, Hu Y, Qi X, Jiang F, et al. Epidemiological characteristics of 2143 pediatric patients with 2019 coronavirus disease in China. Pediatrics. 2020; 145: e20200702.PubMed: https://pubmed.ncbi.nlm.nih.gov/32179660/
- Guerra, F.M, Bolotin S, Lim G, Heffernan J, Deeks SL, et al. The basic reproduction number (R0) of measles: a systematic review. Lancet Infect Dis. 2017; 17: e420-e428. PubMed: https://pubmed.ncbi.nlm.nih.gov/28757186/
- Hamner L, Dubbel P, Capron I, Ross A, Jordan A, et al. High SARS-CoV-2 attack rate following exposure at a choir practice—Skagit County, Washington, March 2020. Morbidity and Mortality Weekly Report. 2020; 69: 6006-610.
- Ehsanifar M. Airborne aerosols particles and COVID-19 transition. Environ Res. 2021; 200: 111752. PubMed: https://pubmed.ncbi.nlm.nih.gov/34302822/
- Fisher KA, Tenforde MW, Feldstein LR, Lindsell CJ, Shapiro NI, et al. Community and close contact exposures associated with COVID-19 among symptomatic adults ≥ 18 years in 11 outpatient health care facilities—United States, July 2020. Morbidity and Mortality Weekly Report. 2020; 69: 1258-1264. PubMed: https://pubmed.ncbi.nlm.nih.gov/32915165/
- Kuderer NM, Choueiri TK, Shah DP, Shyr Y, Rubinstein SM, et al. Clinical impact of COVID-19 on patients with cancer (CCC19): a cohort study. Lancet. 2020; 395: 1907-1918. PubMed: https://pubmed.ncbi.nlm.nih.gov/32473681/
- Ehsanifar M, Rafati M, Wang J. Neurological complications related to COVID-19 infections following exposure to airborne aerosol particles. Clin Res Clin Trials. 2022; 5.
- Inglesby TV. Public health measures and the reproduction number of SARS-CoV-2. JAMA. 2020; 323: 2186-2187. PubMed: https://pubmed.ncbi.nlm.nih.gov/32356869/
- Imai N. Report 3: Transmissibility of 2019-nCoV, WHO Collaborating Centre for Infectious Disease Modelling. MRC Centre for Global Infectious Disease Analysis, J-IDEA, Imperial College London, UK, 2020.
- Alford RH, Kasel JA, Gerone PJ, Knight V. Human influenza resulting from aerosol inhalation. Proc Soc Exp Biol Med. 1966; 122: 800-804. PubMed: https://pubmed.ncbi.nlm.nih.gov/5918954/
- Memoli MJ, Shaw PA, Han A, Czajkowski L, Reed S, et al. Evaluation of antihemagglutinin and antineuraminidase antibodies as correlates of protection in an influenza A/H1N1 virus healthy human challenge model. M Bio. 2016; 7: e00417-00416. PubMed: https://pubmed.ncbi.nlm.nih.gov/27094330/
- Lakdawala SS, Menachery VD. The search for a COVID-19 animal model. Science. 2020; 368: 942-943. PubMed: https://pubmed.ncbi.nlm.nih.gov/32467379/
- Halfmann PJ, Hatta M, Chiba S, Maemura T, Shufang Fan et al. Transmission of SARS-CoV-2 in domestic cats. New Engl J Med. 2020; 383: 592-594. PubMed: https://pubmed.ncbi.nlm.nih.gov/32402157/
- Richard M, Kok A, de Meulder D, Bestebroer TM, Lamers MM, Cet al. SARS-CoV-2 is transmitted via contact and via the air between ferrets. Nature Commun. 2020; 11: 1-6. PubMed: https://pubmed.ncbi.nlm.nih.gov/32641684/
- Ehsanifar M, Yavari Z, Motaghedifar MR, Rezaei M. Risk of activation of human viruses lurking in ambient following COVID-19 prevention supplies excessive use. J Community Med Health Solut. 2022; 3: 011-015. PubMed: https://www.heighpubs.org/jcmhs/jcmhs-aid1014.php
- Yang YExuberant elevation of IP-10, MCP-3 and IL-1ra during SARS-CoV-2 infection is associated with disease severity and fatal outcome. MedRxiv. 2020.
- Sia SF. Pathogenesis and transmission of SARS-CoV-2 in golden hamsters. Nature. 2020; 583: 834-838.
- Coleman CM, Venkataraman T, Liu YV, Glenn GM, Smith GE, et al. MERS-CoV spike nanoparticles protect mice from MERS-CoV infection. Vaccine. 2017; 35: 1586-1589. PubMed: https://pubmed.ncbi.nlm.nih.gov/28237499/
- Gralinski LE, Baric RS. Molecular pathology of emerging coronavirus infections. J Pathol. 2015; 235: 185-195. PubMed: https://pubmed.ncbi.nlm.nih.gov/25270030/
- Xu Z, Shi L, Wang Y, Zhang J, Huang L, et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir Med. 2020; 8: 420-422. PubMed: https://pubmed.ncbi.nlm.nih.gov/32085846/
- Zheng S, Fan J, Yu F, Feng B, Lou B, et al. Viral load dynamics and disease severity in patients infected with SARS-CoV-2 in Zhejiang province, China, January-March 2020: retrospective cohort study. BMJ. 2020; 369:PubMed: https://pubmed.ncbi.nlm.nih.gov/32317267/
- Zhu S, Jenkins S, Addo K, Heidarinejad M, Romo SA, et al. Ventilation and laboratory confirmed acute respiratory infection (ARI) rates in college residence halls in College Park, Maryland. Environ Int. 2020; 137: 105537. PubMed: https://pubmed.ncbi.nlm.nih.gov/32028176/
- Wargocki P, Sundell J, Bischof W, Brundrett G, Fanger PO, et al. Ventilation and health in non-industrial indoor environments: report from a European multidisciplinary scientific consensus meeting (EUROVEN). Indoor Air. 2002; 12: 113-128. PubMed: https://pubmed.ncbi.nlm.nih.gov/12216467/
- Li Y, Qian H, Hang J, Chen X, Hong L, et al. Evidence for probable aerosol transmission of SARS-CoV-2 in a poorly ventilated restaurant. MedRxiv. 2020.
- Miller A, Reandelar MJ, Fasciglione K, Roumenova V, Li Y, et al. Correlation between universal BCG vaccination policy and reduced mortality for COVID-19. MedRxiv. 2020.
- Liu L, Li Y, Nielsen PV, Wei J, Jensen RL. Short‐range airborne transmission of expiratory droplets between two people. Indoor Air. 2017; 27: 452-462. PubMed: https://pubmed.ncbi.nlm.nih.gov/27287598/
- Ehsanifar M. Does Exposure to Air Pollution Fine Particles and COVID-19 Contribute to the Risk of Ischemic Stroke? Health. 2021; 2: 1020.
- Jarvis CI, Zandvoort KV, Gimma A, Prem K, CMMID COVID-19 working group, et al. Quantifying the impact of physical distance measures on the transmission of COVID-19 in the UK. BMC Med. 2020; 18: 1-10. PubMed: https://pubmed.ncbi.nlm.nih.gov/32375776/
- Cowling BJ, Ali ST, Ng TWY, Tsang TK, Li JCM, et al. Impact assessment of non-pharmaceutical interventions against coronavirus disease 2019 and influenza in Hong Kong: an observational study. Lancet Public Health. 2020; 5: e279-e288. PubMed: https://pubmed.ncbi.nlm.nih.gov/32311320/
- Milton DK, Fabian MP, Cowling BJ, Grantham ML, McDevitt JJ, et al. Influenza virus aerosols in human exhaled breath: particle size, culturability, and effect of surgical masks. PLoS Pathog. 2013; 9: e1003205. PubMed: https://pubmed.ncbi.nlm.nih.gov/23505369/
- Leung NH, Chu DKW, Shiu EYC, Chan KH, McDevitt JJ, et al. Respiratory virus shedding in exhaled breath and efficacy of face masks. Nature Med. 2020; 26: 676-680. PubMed: https://pubmed.ncbi.nlm.nih.gov/32371934/
- Xiao F, Sun J, Xu Y, Li F, Huang X, et al. Infectious SARS-CoV-2 in feces of patient with severe COVID-19. Emerg Infect Dis. 2020; 26: 1920. PubMed: https://pubmed.ncbi.nlm.nih.gov/32421494/
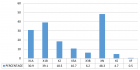
Figures:
Figure 1
Similar Articles
-
Indoor air pollution and behavioral factors affecting to COVID-19 transitionMojtaba Ehsanifar*,Mehravar Rafati,Zeinab Yavari. Indoor air pollution and behavioral factors affecting to COVID-19 transition. . 2022 doi: 10.29328/journal.jcmhs.1001015; 3: 016-020
Recently Viewed
-
Bee venom: a case of effectiveness on skin varicosities veins with review of its dermatological benefitsMohamed El Amraoui*,Rachid Frikh,Naoufal Hjira,Mohammed Boui. Bee venom: a case of effectiveness on skin varicosities veins with review of its dermatological benefits. Ann Dermatol Res. 2020: doi: 10.29328/journal.adr.1001010; 4: 006-008
-
ERRATUM to: Fiesta vs. Stress Condition the Incidence and the Age at Menarche. Forty Years of ResearchCarlos Y. Valenzuela*. ERRATUM to: Fiesta vs. Stress Condition the Incidence and the Age at Menarche. Forty Years of Research. Clin J Obstet Gynecol. 2025: doi: 10.29328/journal.cjog.1001190(E); 8:
-
Transnasal Humidified Rapid-Insufflation Ventilatory Exchange (THRIVE) in High-Risk Endoscopic Procedures: A Non-Intubation ApproachNaba Madoo*,Vaibhavi Baxi. Transnasal Humidified Rapid-Insufflation Ventilatory Exchange (THRIVE) in High-Risk Endoscopic Procedures: A Non-Intubation Approach. Int J Clin Anesth Res. 2025: doi: 10.29328/journal.ijcar.1001033; 9: 035-036
-
Seasonal Influenza in MoroccoSafae El-Kochri,Nadia Touil,Rachid Abi,Hajar Cherkaoui Malki,Mohammed Rida Tagajdid,Hicham Elannaz,Zhor Kassmi,Fadoua Amraoui,Yassine Benaissi,Youssef Addi,Ahmed Reggad,Mohammed Elqatni,Bouchra Machichi,Abdelilah Laraqui A,Elarbi Bouaiti E,Khalid Ennibi,Idriss Lahlou Amine. Seasonal Influenza in Morocco. Int J Clin Virol. 2025: doi: 10.29328/journal.ijcv.1001065; 9: 021-027
-
Obstetric Paradoxes and Didactic Equations: The Impact of Mathematical Teaching on Childbirth and BeyondPascual Chiago*. Obstetric Paradoxes and Didactic Equations: The Impact of Mathematical Teaching on Childbirth and Beyond. Clin J Obstet Gynecol. 2025: doi: 10.29328/journal.cjog.1001197; 8: 096-101
Most Viewed
-
Feasibility study of magnetic sensing for detecting single-neuron action potentialsDenis Tonini,Kai Wu,Renata Saha,Jian-Ping Wang*. Feasibility study of magnetic sensing for detecting single-neuron action potentials. Ann Biomed Sci Eng. 2022 doi: 10.29328/journal.abse.1001018; 6: 019-029
-
Evaluation of In vitro and Ex vivo Models for Studying the Effectiveness of Vaginal Drug Systems in Controlling Microbe Infections: A Systematic ReviewMohammad Hossein Karami*, Majid Abdouss*, Mandana Karami. Evaluation of In vitro and Ex vivo Models for Studying the Effectiveness of Vaginal Drug Systems in Controlling Microbe Infections: A Systematic Review. Clin J Obstet Gynecol. 2023 doi: 10.29328/journal.cjog.1001151; 6: 201-215
-
Causal Link between Human Blood Metabolites and Asthma: An Investigation Using Mendelian RandomizationYong-Qing Zhu, Xiao-Yan Meng, Jing-Hua Yang*. Causal Link between Human Blood Metabolites and Asthma: An Investigation Using Mendelian Randomization. Arch Asthma Allergy Immunol. 2023 doi: 10.29328/journal.aaai.1001032; 7: 012-022
-
Impact of Latex Sensitization on Asthma and Rhinitis Progression: A Study at Abidjan-Cocody University Hospital - Côte d’Ivoire (Progression of Asthma and Rhinitis related to Latex Sensitization)Dasse Sery Romuald*, KL Siransy, N Koffi, RO Yeboah, EK Nguessan, HA Adou, VP Goran-Kouacou, AU Assi, JY Seri, S Moussa, D Oura, CL Memel, H Koya, E Atoukoula. Impact of Latex Sensitization on Asthma and Rhinitis Progression: A Study at Abidjan-Cocody University Hospital - Côte d’Ivoire (Progression of Asthma and Rhinitis related to Latex Sensitization). Arch Asthma Allergy Immunol. 2024 doi: 10.29328/journal.aaai.1001035; 8: 007-012
-
An algorithm to safely manage oral food challenge in an office-based setting for children with multiple food allergiesNathalie Cottel,Aïcha Dieme,Véronique Orcel,Yannick Chantran,Mélisande Bourgoin-Heck,Jocelyne Just. An algorithm to safely manage oral food challenge in an office-based setting for children with multiple food allergies. Arch Asthma Allergy Immunol. 2021 doi: 10.29328/journal.aaai.1001027; 5: 030-037

If you are already a member of our network and need to keep track of any developments regarding a question you have already submitted, click "take me to my Query."