More Information
Submitted: 17 November 2020 | Approved: 04 December 2020 | Published: 07 December 2020
How to cite this article: Oluwasusi JO, Thomas KA, Olujide MG, Oluwasusi YO. Utilization of midwives service scheme among women farmers in Southwestern Nigeria. J Community Med Health Solut. 2020; 1: 035-046.
DOI: 10.29328/journal.jcmhs.1001005
Copyright License: © 2020 Oluwasusi JO, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Women farmers; Skilled birth attendants; Child bearing; Maternal mortality
Utilization of midwives service scheme among women farmers in Southwestern Nigeria
Oluwasusi JO1*, Thomas KA2, Olujide MG2 and Oluwasusi YO3
1Department of Agricultural Science, Afe Babalola University, Ado-Ekiti, Ekiti State, Nigeria
2Department of Agricultural Extension & Rural Development, University of Ibadan, Ibadan, Nigeria
3Department of Vocational Training, College of Forestry, Ibadan, Nigeria
*Address for Correspondence: Oluwasusi JO, Department of Agricultural Science, Afe Babalola University, Ado-Ekiti (ABUAD), P.M.B 5454, Ado-Ekiti, Ekiti State, Nigeria, Email: [email protected]; [email protected]
Maternal mortality accounts for most deaths in agrarian communities of Nigeria due to poor access to midwives services and inadequate Skilled Birth Attendants (SBAs). The Midwives Service Scheme (MSS) was established to engage more SBAs and advocate better utilization of pre and post-natal care services. Studies have focused on maternal mortality reduction, however, information on underlying factors that predispose MSS target beneficiaries to its utilization is scarce. Therefore, utilization of MSS among women farmers in southwestern Nigeria was investigated. A four-stage sampling procedure was used. Three states from southwestern states (Oyo, Ogun and Ekiti) were randomly selected. Thereafter, ten Local Government Areas (LGAs) from eighteen LGAs that adopted MSS programme in the selected states were sampled. Also, 30% of the MSS facilities in the sampled LGAs were selected, resulting in 13 MSS facilities. Proportionate sampling technique was used to select 20% of registered women farmers in the selected 13 MSS facilities to give 207 respondents. Interview schedule was used to collect data on respondents’ socioeconomic characteristics, Maternal Health Information Sources (MHIS), Maternal Health Information Seeking Behavior (MHISB) and utilization of MSS. Data were analyzed using descriptive and inferential statistics. About (55.6%) of the respondents had formal education. MHISB and effectiveness of MSS was rated low by 53.2% and 55.6% of the respondents, respectively. MSS was moderately utilized by 64.7% of the respondents. The MSS utilization was 49.24 ± 11.39 (Oyo), 45.08 ± 9.28 (Ogun) and 44.00 ± 10.71 (Ekiti). Respondents’ education (χ2 = 12.85), family size (r = 0.02), monthly income (r = 0.48) related positively and significantly (r = 0.27) to MSS utilization.
The society is sustained on continuous governments’ investment in her population’s health, skills, knowledge and better practices protected by laws and policies. Family institution remains the basic social institution in the society, formed on marriage, celebrated with pregnancy and childbirth for the preservation of human relationships and generation of manpower needed for the development of communities. However, maternity in rural area is confronted with serious traditional practices and norms putting women farmers at risk of maternal mortality in agrarian societies of the world. Pregnant women’s tendency for safe child delivery depends on the competency and assistance of skilled birth attendants sought during childbirth. However, there is a rural-urban variation in the records of safe child delivery and maternal mortality in the country due to large concentration of obstetrics and gynecologists with the best expertise in safe child delivery concentrated at the urban areas. The urban areas have the secondary and tertiary health facilities, while the rural areas are equipped with few trained midwives co-existing with traditional birth attendants [1].
In addition, high maternal death during pregnancy and childbirth is generally a serious health concern in less advanced nations, including Nigeria [2]. Moreover, it was reported that an estimate of over 300,000 women died during pregnancy and childbirth, with virtually all the maternal deaths recorded in poor health facilities and majority would have been averted [3]. Yearly, thousands of Nigerian women die from pregnancy and childbirth cases, often marked with circumstances of poor medical attention [4]. Studies accounted that most of these unpleasant cases could be forestalled and curtailed if childbearing female folks registered in, and utilized modern health facilities equipped with skilled birth attendants during their pregnancy period, child delivery state and post child delivery [5-7]. Women seem to die more during pregnancy and childbirth in the rural areas than the urban areas [8].
Rural women are possibly subjected to primitive conditions that seem to promote the patronage of traditional birth attendance to child deliveries at homes and spiritual places in a bid to preserve families’ cultural heritage and ethos that are unconsciously done as harmful childbirth practice. These may aggravate rural women’s vulnerability to maternal mortality. The health of rural mothers is not only crucial to the health and survival of the children, but sustains their tremendous contributions to rural economies and national development. Women dominate the rural population, where majority of Nigerians live and farm [9]. Furthermore, Aina, [10] posited that women in rural areas are typical farmers and artisans, who also delve into diverse entrepreneurial occupations. Women largely farm, process and ensure the sales of farm produce in almost all African nations [11].
According to United Nations Children Education Fund (UNICEF) report of 2014, women and child death pattern presented that Nigeria had not been improving rapidly to meet up with the world developmental objectives. Successive governments have adopted various programmes on safe motherhood, with many being initiated by non-governmental organizations attracting funding from international donors that are less sustainable, as withdrawal of sponsorship is inevitable after sometime; resulting in reduction in maternal death [12,13]. This reduction in maternal death in Nigeria, according to Okonofua, et al. [14] still remains one of the worst records of women’s death due to child bearing. The need to promote sustainable safe maternal health and expanded access to skilled birth attendants in Nigeria, particularly the rural communities, notable for inadequate basic amenities and underserved skilled birth attendance to child bearing women, led to governments’ establishment of Midwives Service Scheme (MSS) by the 2009 Appropriation Act under the coordination and supervision of the National Primary Health Care Development Agency (NPHCDA).
Nigeria government launched Midwives Service Scheme in 2009, as a responsive policy to the concern of non-sustainability in the reduction of maternal death drive in the country. The MSS was established under the Federal Ministry of Health to promote equitable maternal health services and increase women’s access to skilled birth attendants in both urban and rural areas of the country. The MSS programme is structured by the seal of memorandum of understanding among the three-tiers of government in Nigeria, shouldering the responsibilities for primary health care in Nigeria, under the watch of the National Primary Health Care Development Agency (NPHCDA).
In all the PHC facilities, a Village Development Committee (VDC) and Ward Development Committee (WDC) are made up of influential people and elected representatives of the people in the community. They are established to enhance community participation and ownership of the MSS by the people in the MSS resident communities. Despite the establishment of MSS by the collaboration of federal, state and local governments in Nigeria in 2009, as a possible effort to salvage maternal mortality in the country with many primary health centres sited and utilized in the rural areas as midwives service scheme facilities, little progress seems to be achieved. Mojekwu and Ibekwe [15] stated that women death pattern to childbirth is still high in Nigeria, having one of the highest accounts of global women deaths, without a definite period of relief. It is against this backdrop that the study determined the utilization of MSS among women farmers in southwestern Nigeria. This study therefore looked into the following research objectives:
The general objective of the study was to determine the midwives services scheme utilization among women farmers in south western, Nigeria.
The specific objectives of the study are to:
1. Examine the maternal health information sources available to the women farmers in the study area?
2. Investigate the maternal health information seeking behavior of the women farmers to maternal health services under MSS in the study area?
3. Determine the level of utilization of midwives services scheme utilization by the respondents in the study area.
Hypotheses of the study
Ho1: There is no significant relationship between respondents’ socioeconomic characteristics and the utilization of midwives service scheme.
Ho2: There is no significant relationship between effectiveness of midwives service scheme by the respondents and the utilization of the midwives service scheme.
Ho3: There is no significant difference in the level of midwives service scheme utilization among the respondents across the sampled states.
Theoretical framework
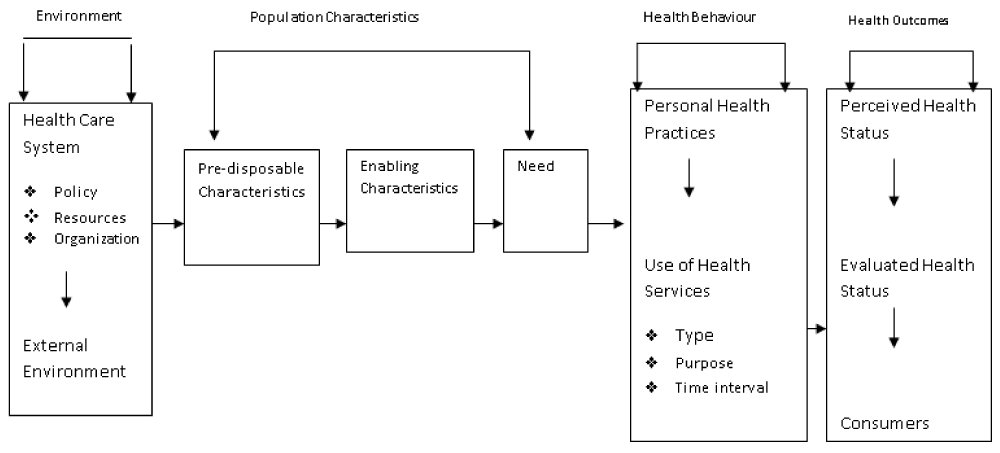
Andersen model of health care utilization: Andersen, [16] developed a model of health care utilization which considers three levels of decisive factors affecting outcomes (Figure 1).
Figure 1: Schematic representation of Andersen’s Model of Health Services Utilization Source: Andersen (1995).
(i) Predisposing factors: These represent the influencing elements to utilize health care services. An individual is more or less likely to use health services based on his or her socioeconomic characteristics and belief in the benefits of health services. The predisposing factors include age, gender, marital status, education, occupation, societal norm and membership of an organization, which could determine the social and economic class of a person in a community, his or her ability to cope with the health problem at hand and the resources available to deal with the problem. General beliefs or attitudes about health care services might also predict its use. An individual who believes health care services are useful for the treatment of ailing conditions will likely utilize those services for his or her sick conditions.
(ii) Enabling factors: This includes available infrastructural amenities and economic potentials in an environment, access to health facilities and awareness on health services. Accessibility to health care facilities involves proximity to the health care facilities and the availability of health professions to attend to patients’ health needs.
(iii) Need based factors: This includes individuals’ perception of need for health services, whether personally or socially influenced disposition to health needs. Thus, health service need could either be an individual’s subjective assessment of need or advised need offered by health professional. Andersen health model was revised in 1995, showing that utilization of health care system depends on health policy, social and economic accessibility to health care services, and conviction over time. It also shows that there is a connective association among processing factors such as; primary determinants, health behaviors and health outcomes which lead to utilization of health services among people.
Primary determinants are the factors influencing health behaviors, which include demographics, the management of the health care system and the external environment, characterized by traditions, infrastructural facilities and economic factor influencing the utilization of health facilities and services. Management of health care system involves health personnel and medical equipment supplies, likewise level of funding. These ultimately influence individuals’ behaviors toward health services utilization.
Area of study
The study was conducted in Southwestern Nigeria. It is one of the six geopolitical zones of Nigeria. The zone comprises of Lagos, Oyo, Ogun, Ondo, Osun and Ekiti states. There are lot of villages in the Southwestern Zone of the country. The basic infrastructure needed to drive socioeconomic growth and health development is in poor condition. The primary occupation of the people is farming, with great involvement of women as a key driver in the various aspects of agricultural practices, transportation and distribution to the local markets. The women are also involved in animal husbandry and petty trading activities. Traditional rulers and opinion leaders exert great influence on the people’s response and involvement in intervention programmes. This area was chosen because of the similarity in the cultural language, climatic, environmental, political and socioeconomic factors. It has latitude of 50 South, 90 North and Longitude of 20 and 80 East, it shares boundary with Atlantic Ocean in the South, River Niger in the East, Republic of Benin in the West and North-Central Nigeria in the North; likewise a land area of 78,505.17 square kilometres [17]. National census of 2006 has South West Nigeria to be populated by 27, 722, 432 people.
Sampling procedure and sample size
A four-stage sampling procedure was adopted for this study. The first stage involved a simple random selection of 50% of the Southwestern states (Oyo, Ogun and Ekiti). Respondents were drawn from the list of registered child bearing women in MSS, onward of 2 to 9 months after child delivery in each of the selected states.
Sources and instruments of data collection
Both qualitative and quantitative methods were used to collect data from the respondents. The data were obtained with the use of structured interview schedules. The study also employed Focus Group Discussions (FGD) with the women farmers and In-depth interviews (IDIs) with Key Informants from the Village Development Committee for qualitative data.
Measurement of variables
Socioeconomic characteristics of child bearing women were measured at interval and nominal levels. Maternal health information sources of the respondents were sought through a list of sources of information on maternal health presented to respondents on a 2-point scale of yes and no with scores of 2 and 1, respectively. The frequency of information sourcing was sought on a 3- point scale of Always, Occasionally and Never with scores of 3, 2 and 1, respectively. Respondents’ maternal information seeking behaviour towards MSS utilization was sought on a 3-point scale of early promptly sought, delayed sought and reliance on traditional birth attendants for maternal attention with scores of 3, 2 and 1, respectively. Minimum score of 16 and maximum score of 48 were recorded based on their responses. Mean score was obtained as 37.9 ± 7.83 and respondents with score below the mean was categorized as having low maternal information-seeking behavior towards MSS utilization while mean and above was categorized as high maternal information-seeking behavior towards MSS utilization. Effectiveness of MSS utilization by the respondents was measured on a 3-point scale of highly effective, effective and not effective with scores of 3, 2 and 1, respectively. Level of effectiveness of MSS was determined by pooling the scores from the effectiveness scale as indicated by each of the respondents, the mean score of 17.63 ± 5.34 was obtained and used to categorize respondents into high and low levels of effectiveness of MSS. The minimum and maximum scores obtainable were 10.00 and 30.00, respectively. Respondents’ utilization of MSS was measured on a 3-point scale of always, rarely and never with scores of 2, 1 and 0, respectively. Level of utilization was determined by pooling the scores from the utilization scale as indicated by each of the respondents, the mean score of 46.42 ± 10.80 was obtained and used to categorize respondents into high and low levels of utilization. Minimum score of 30 and maximum score of 72 were recorded based on their responses.
Analysis of data
Data were described with the use of descriptive statistics such as the means, frequencies and percentages. Tests of hypotheses were carried out for hypothesis 1 using Chi-square and Pearson Product Moment Correlation (PPMC). Hypothesis 2 was tested using PPMC, while hypothesis 3 was tested using Analysis of variance (ANOVA).
Socioeconomic characteristics of respondents
The mean age, 34.97 ± 8.20, as shown in table 1, confirms that women farmers in the study area were in their young adulthood and economically active age. This implies that majority of the respondents were in their productive and child bearing age with some level of vulnerability to maternal death, which is expected to awaken their consciousness to utilising safe maternal health in the stance of midwives service scheme. This finding is in consonance with the report of Vos, et al. [18] which reveal that young childbearing women are more at risk of maternal death. Table 2 further reveals that the average family size was 6.70 ± 1.50 members. The average family size across the selected area was relatively large in size. This implies high childbirth record, with little or low safe contraceptives use, among the rural women-farmers. This result therefore suggests that women farmers place high premium on child birth, as a means of driving farm labour in the study area. The result is consistent with Ayoade, [19] which reported a family size of more than 7 members among farm families in Oyo State, thereby providing family labour for agricultural operations.
| Table 1: Sampling of child bearing women farmers utilising MSS facilities. | |||||
| 50% of Southwestern States | Adopted LGAs for MSS have 4 facilities respectively | 50% of Sampled LGAs | 30% of the MSS facilities in each of the sampled LGAs | Registered women farmers in the MSS facilities | 20% of Sampled Women farmers |
| OGUN | 5 | 3 LGAs (Ipokia, Obafemi Owode and Odogbolu) |
4 Ipokia {Ijonfin}, Obafemi Owode {Ofada and Mokoloki}, Odogbolu {Mabalufo} | 312 | 62 |
| OYO | 8 | 4 LGAs (Ibarapa, Atisbo, Surulere and Iwajowa) |
5 Ibarapa{Maya and Okemole},Atisbo{Ofiki}Surulere {Gambari}, Iwajowa {Ijio} | 416 | 83 |
| EKITI | 5 | 3 provinces (Aramoko, Ode and Ikere) |
4 Aramoko {Ara}, Ode {Imojo}, Ikere{Oke Emure and Okeyard} | 309 | 62 |
| Table 2: Distribution of respondents by socioeconomic characteristics in the study area. | ||
| Socioeconomic Characteristics | Frequency (207) | % |
| Age < 20 years 21-30 years 31-40 years 41-50 years Above 50 years |
7 54 82 61 3 34.97 years ± 8.20 |
3.4 26.1 39.6 29.5 1.4 |
| Family size 1-3 4-6 7-9 |
9 91 107 6.70 persons ± 1.50 |
4.3 44.0 51.7 |
| Primary Occupation Crop Farming Livestock Rearing Crop Farming & Livestock Agricultural Processing |
116 10 5 76 |
56.0 4.8 2.4 36.7 |
| Secondary Occupation Agricultural Processing Trading Craft Making |
71 120 16 |
34.3 58.0 7.7 |
| Years of farming Less or equal 10 years 11-20 years 21-30 years 31-40 years 40-50 years |
6 53 99 40 9 22.14 years ± 9.04 |
2.9 25.6 47.8 19.3 4.3 |
| Estimated Monthly Income ≤ ₦20,000 ₦21,000-₦40,000 ₦41,000-₦60,000 ₦61,000-₦80,000 |
103 85 17 2 ₦22,014.43 ± 13.08 |
49.8 41.1 8.2 1.0 |
| Membership of Association Cooperative Society Occupational Group Religious Group |
92 104 11 |
44.4 50.2 5.3 |
The study also reveals that more than half (56.0%) of the women farmers were crop farmers and 36.7% were processors. This is further supported by the report of Ayoade, [19] that women are well involved in food production to sustain their families’ welfare.
Table 2 further reveals that more than half (58.0%) of the women farmers engaged in trading of agricultural commodities and forest products during on-season and off-season as secondary occupation. This implies that secondary occupation could offer additional sources of revenue to the respondents, improve their opportunity of having control over free decision and responsibility to utilize safe maternal health programme of MSS. This finding is in consonance with Edna, et al. [20] who reported that agricultural practices cannot effectively meet the social and economic needs of the subsistent farmers; secondary occupations therefore appropriately buffer their farm income.
The study assessed the years of farming in table 2 to be an average of 22.14 ± 9.04 years. The years of farming reflect an index of farming experience. Women farmers with longer years of farming experience stand better chances of having better farming, farming risk management skills and knowledge of profitable farming. Nwaobiola and Onumadu, [21] work supported this finding that farming experience advances the productivity of farmers through open-mindedness to technology adoption, which in the same vein improves their farm yield. The finding is also in consonance with the findings of Nwaogwu, et al. [22] who reported that farming experience aids farmers’ timely innovation adoption and enhances the profitability of farm venture. The mean monthly income of ₦22,014.43 ± 13.08 as shown in table 2 confirms that women farmers in the study area were small holder farmers with low income even with their complementary earnings from off-farm and non-farm activities as secondary occupation. This indicates that the economies of primary farming operations and combined secondary occupations were small, yielding low monthly income, which could limit respondents’ utilization of MSS. This finding is supported by Adamu, [23] who reported that family income is an indicator to utilize modern health care facilities, hence it predicates the financial capacity and responsibility of bearing the cost of medical service.
Table 2 reveals that 44.4% of the respondents across the selected states belonged to cooperative group, while 50.2% belonged to occupational group. This means that the women farmers were privileged to receive and share information on agricultural production and safe maternal health through these social organizations. The finding is also in consonance with Hagedoorn, [24] who reported that social relationships increase awareness of better practices and making informed decisions on recognized needs. This finding also corroborates Adekoya, [25] who asserted that membership of associations promotes symbiotic relationship and understanding among farmers, which often result into dedication to assist each other.
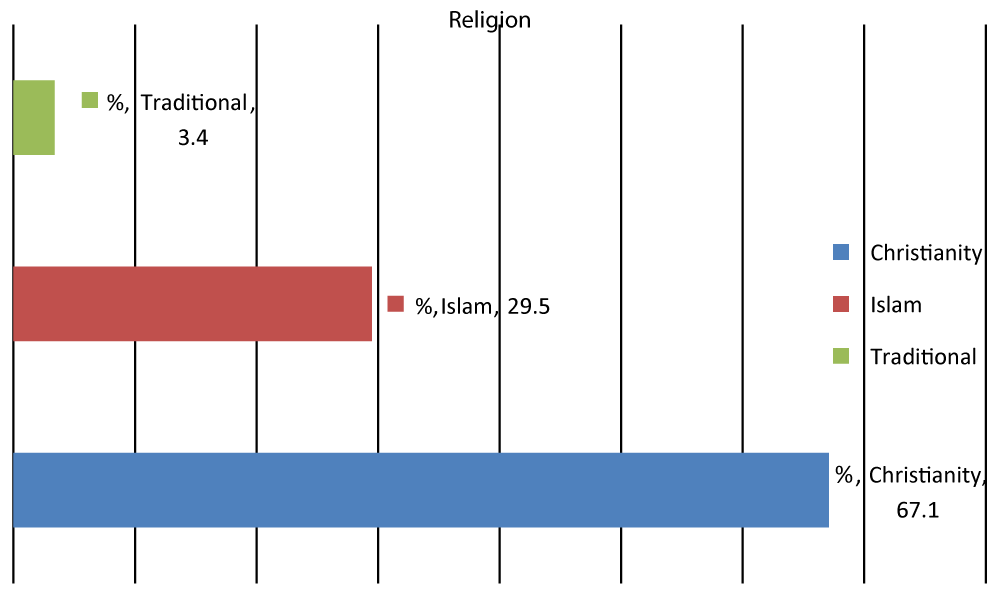
Religion is reported in figure 2 as an integral part of people’s way of life, premised on belief, custom, moral and habits that sharpen the minds of people in the face of various life events and challenges, transmissible from generation to generation. All the three main religion groups were represented in the study area, with the result, reflecting that most (67.1%) were Christians, 29.5% were Muslims and very few (3.4%) of the respondents were traditionalists. This implies that religion among the respondents is a powerful tool and endorsement platform to seek preventive health care through MSS utilization, as it does not contradict the utilization of MSS services.
Figure 2: Percentage distribution of the respondents’ religion.
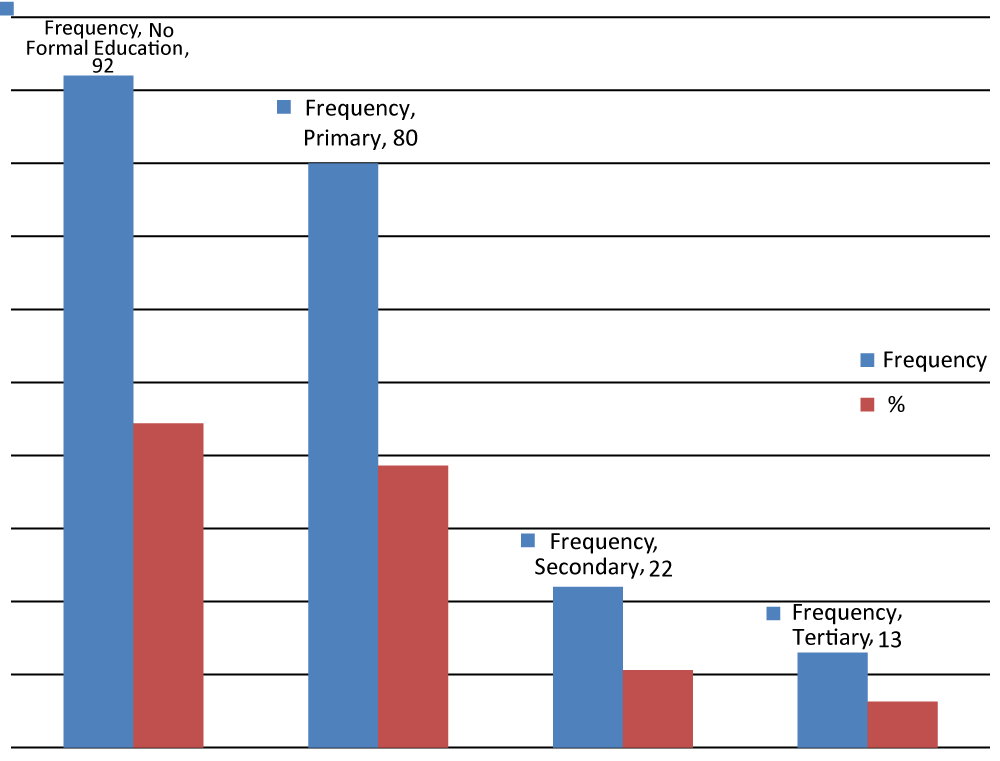
Educational status of respondents
The study reveals in figure 3, that 44.4% of the respondents had no formal education, while more than half (55.6%) had a form of formal education across the study area. This implies that many of the women farmers had a level of formal education. This could be connected to parents in the selected area, giving at least primary education to many of their girl children before giving them out to men in marriage. This infers that educated women are more likely to access safe maternal health information from diverse sources, disseminate to others and use, just in the case of MSS for mother and child safety. This result negates the assertion of Oluwadare and Jegede, [26] who reported that daughters are restricted to demeaning traditions that deny them access to schooling, financial resources and making independent decisions on their life aspirations. This finding is also corroborated by the assertion of Fasokun, et al. [27] that education guarantees enlightenment and liberty of people of all ages from ignorance and deprivations of human right, particularly women as it offers them capacity and free choice to make appropriate decisions on life issues.
Figure 3: Percentage distribution of respondents’ educational status.
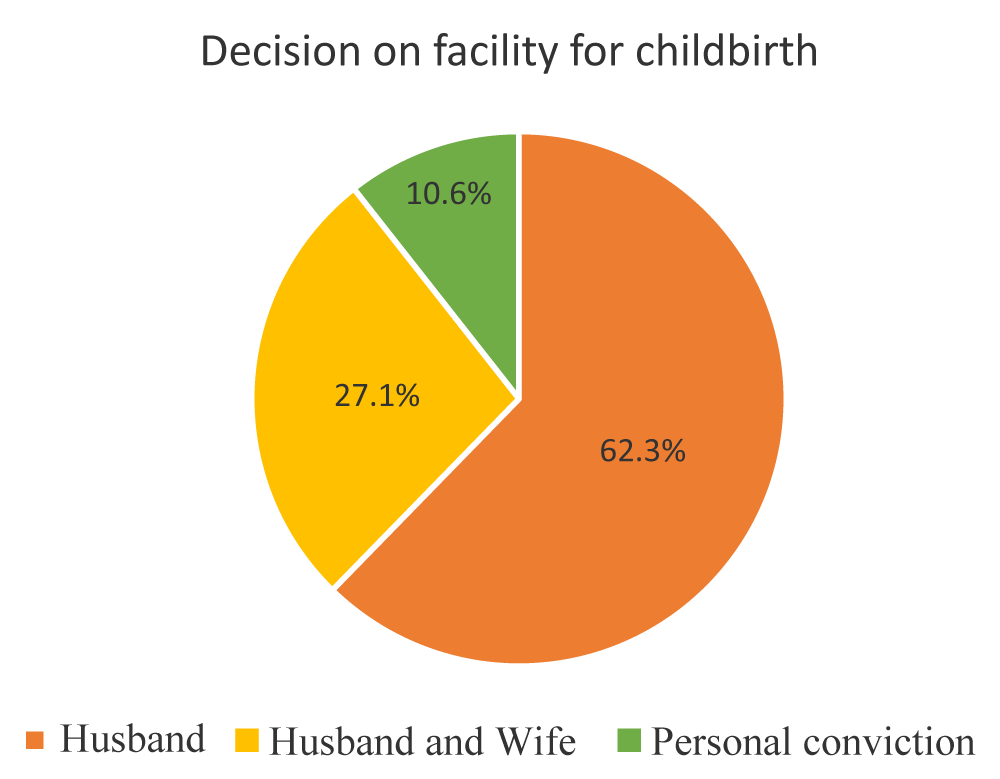
Decision making on facility for childbirth
The study reveals in figure 4, that husband decided the facility for child birth (62.3%) across the selected study areas, while 27.1% of the facility used by women farmers for childbirth was decided by husband and wife. This implies that husband influenced respondents’ decision on health facility for childbirth and largely owned responsibility on the decision concerning facility for child delivery. WHO, [28] supported this finding that women’s decision on their reproductive health is subject to consent and approval of their husbands.
Figure 4: Percentage distribution of respondents on decision making concerning facility for childbirth.
FDG excerpts with men in the Village Development Committee at Orun Ekiti supported this finding that,
“Men are the heads of their families and decisions concerning all members of the family are principally taken by men. The same thing applies to MSS utilization in families, but for efforts of the group in talking with the men to allow the participation of their pregnant wives in the MSS programme with proofs of many safe children deliveries in our MSS centre for over eight years now, it has been allowing more registration of pregnant women in the programme and utilization of MSS in our community.”
Maternal health information sources available to the respondents
Sources of respondents’ maternal health information.
Table 3 shows that community health extension workers (96.1%) were the major source of maternal health information to the respondents. This was buttressed in the FGD reports that respondents preferred and used community health extension workers most for their maternal health information,
“because we usually hear of the best and safest child birth practices, children care and other maternal health information and the importance of adherence to them through community health extension workers, who don’t get tired of visiting our homes”.
| Table 3: Distribution of respondents based on sources of maternal health information (N = 207). | |||
| Sources of maternal health information | Frequency 207 | (%) | Rank |
| Community Health Extension Workers Midwives Radio Village Development Committee (VDC) Traditional birth attendants Friends Religious Group Occupational Group Television Fliers |
199 176 161 157 129 32 13 10 8 4 |
96.1 85.0 77.8 75.8 62.3 15.5 6.3 4.8 3.9 1.9 |
1st 2nd 3rd 4th 5th 6th 7th 8th 9th 10th |
Other varieties of media were also sourced by the respondents for appropriate maternal health information on their maternal health needs. Babalola and Fatusi, [29] supported this finding that sourcing maternal health through mass media promotes safe motherhood and corrects existing misconception surrounding reproductive health in the society.
Respondents’ maternal health seeking behavior
Majority (93.7%) of the respondents promptly sought vaccination against and treatment of diseases like measles and pneumonia in infants through MSS. This indicates that women farmers gave priority to the survival of their infants by promptly seeking safe maternal assistance for the survival of their infants, which would transit to dependable cheap family labour in the nearest future. Majority (93.2%) of the respondents sought survival interventions like Vitamin A and de-worming promptly for their infants. This indicates that majority of the respondents gave high premium to child safety through vaccination of their children against diseases and preventing them from worms’ attack that could limit their growth and life potentials through prompt consult of MSS. These findings are consistent with that of Anastasia and Marie, [30] who found that women’s search for reproductive health depends on its reach and publicity to them, which aid their capacity to utilize.
Level of respondents’ maternal health information seeking behavior in MSS facilities
Table 4 reveals that respondents’ maternal health seeking behavior in MSS facilities was low across the study area, with 53.2% having a mean score of less than 38, belonging to the low category. This indicates that the respondents’ maternal information seeking behavior in MSS was low despite many of them having a form of formal education and contacts with community health extension workers in the earlier reports presented in table 2, respectively. This finding is consistent with that of Zhao, et al. [31] that the right maternal information is crucial to safe motherhood and wellbeing of women.
| Table 4: Distribution of respondents based on level of their maternal health information seeking behaviour in MSS facilities. | |||||
| Level of respondents maternal health seeking behaviour towards MSS utilization | (%) | Minimum | Maximum | Mean | SD |
| Low | 53.2 | 20.00 | 48.00 | 37.93 | 7.83 |
| High | 46.8 | ||||
Utilization of MSS
Table 5 shows the services offered by MSS to the respondents. Neonatal care was the most utilized skilled birth attendants service ( = 1.70) as a component of MSS by the respondents. This implies that assistance of skilled birth attendants was well sought and utilized after the delivery of their children by the women farmers while the least utilized skilled birth attendant service accessed by the women farmers was ambulance service ( = 0.40). These suggested that upon respondents safe children delivery and stress underwent, they were very concerned and did their best to keep their children safe unlike utilizing ambulance service that were not readily available and functional in emergency situations. Okwa, [32] supported these findings that women’s use of orthodox health has a bearing to the treatment given them, incremental access and proximity to the facilities around them.
| Table 5: Distribution of Respondents Based on the Utilization of Midwives Service Scheme. | |||||
| Components of mss | Always (%) | Rarely (%) | Never (%) | Rank | |
| Neonatal care Cutting of the umbilical cord safely Safe care of the navel against infection of diseases Provision of warmth to infants Grand Mean |
90.3 96.6 97.6 |
5.8 3.4 2.0 |
3.9 0.0 0.5 |
1.19 1.93 1.97 1.70 |
1st |
| Post natal care Advice on early initiation of breast feeding and how to make non-early lactating mothers lactate Blood pressure and Packed Cell Volume (PCV) as blood level check Weighing of infants Grand Mean |
63.3 70.5 56.5 |
36.2 28.9 42.9 |
0.5 0.5 0.5 |
1.97 1.55 1.56 1.69 |
2nd |
| Skilled birth attendants Attendance to all my pregnancy complaints Assistance of midwives in child delivery Health talk on nutrition education, exclusive breast feeding, stress management and drugs prescribed Grand Mean |
63.8 67.6 67.1 |
36.2 32.4 32.9 |
0.0 0.0 0.0 |
1.63 1.67 1.66 1.65 |
3rd |
| 24 hours qualified management service Child delivery service Care of pregnant women Care of mother and child Grand Mean |
81.6 66.7 63.8 |
18.4 33.3 36.2 |
0.0 0.0 0.0 |
1.82 1.67 1.41 1.57 |
4th |
| ANTENATAL CARE Physical examination of blood pressure and scan Prevention and treatment of malaria Provision of routine drugs and supplements like folic acid and vitamin C Grand Mean |
52.2 54.6 27.5 |
47.3 44.9 71.9 |
0.5 0.5 0.5 |
1.52 1.54 1.27 1.44 |
5th |
| Infant welfare Treatment of minor ailments like malaria and diarrhea Management of childhood diseases like convulsion and measles Treatment of minor injuries Grand Mean |
40.1 59.4 28.9 |
59.9 40.1 70.0 |
0.0 0.5 1.0 |
1.40 1.39 1.28 1.36 |
6th |
| Outreach service Enlightenment and mobilisation campaign for pregnant women in the community Immunisation of children on house to house basis Grand Mean |
78.3 17.9 |
17.9 79.2 |
3.9 2.9 |
1.43 1.35 1.35 |
7th |
| Immunisation Immunisation of mothers against disease like tetanus Immunization of children against diseases like polio and pneumonia Provision of child survival interventions like de-worming and vitamin A Grand Mean |
23.2 21.3 19.8 |
74.9 78.7 80.2 |
2.0 0.0 0.0 |
1.64 1.16 1.21 1.34 |
8th |
| Family planning Counseling on child spacing Counseling on Family planning methods Birth and Emergency plan Grand Mean |
60.4 38.2 43.9 |
39.1 60.9 55.1 |
0.5 1.0 1.0 |
1.28 1.38 1.37 1.34 |
9th |
| Laboratory service Ultrasound scan Malaria and other suspicious diseases check Grand Mean |
0.0 2.22 |
70.0 74.8 |
29.9 2.9 |
1.08 1.19 1.16 |
10th |
| Referral service Identification of required conditions for referral to general and tertiary hospitals by SBAs Management of pregnancy complications Follow up on referral cases to the general and tertiary hospitals Grand Mean |
13.0 14.5 10.1 |
24.2 21.7 23.7 |
62.8 63.7 66.2 |
0.50 0.52 0.44 0.48 |
11th |
| Ambulance service Standby ambulance service Functional ambulance service Non-expensive ambulance service Grand Mean |
7.7 8.2 9.2 |
23.7 23.2 22.2 |
68.6 68.6 68.6 |
0.39 0.41 0.39 0.40 |
12th |
| Field Survey, 2019 *= Mean | |||||
Level of utilization of MSS
The study reveals on table 6 that many (64.7%) of the women farmers’ utilized MSS moderately, having utilized MSS more than the average of 46.42 ± 10.80. This indicates that many of the women farmers did not fully engage the use of MSS to maximize its potentials of preventing maternal death, ensuring safe child birth and ensuring survival of healthy children. Thus, respondents’ low accessibility to MSS, poor effectiveness of MSS operations, low affordability of MSS and prevailing husbands’ decision on child birth in the rural areas earlier reported could be responsible for their inadequate utilization of MSS, which could lead to negative maternal outcomes. This finding corroborates World Health Organization [6,28] that women die of pregnancy and childbirth as a result of low utilization of orthodox medicine. The result is further corroborated by [33] who reported that low accessibility to and utilization of orthodox medical services is laden with patterns of social relationships and interactions, women’s stake in family matters and financial status of families.
| Table 6: Level of Utilization of MSS. | ||||||||
| Levels of Utilization of MSS | Overall | Oyo | Ogun | Ekiti | Minimum | Maximum | Mean | SD |
| Low (30.0-36.5) | 15.5 | 22.9 | 22.6 | 45.2 | 30.00 | 72.00 | 46.42 | 10.80 |
| Moderate (36.6-57.1) | 64.7 | 61.4 | 59.7 | 33.9 | ||||
| High (57.2-72.0) | 19.8 | 15.7 | 17.7 | 20.9 | ||||
| Source: Field Survey, 2019 | ||||||||
Effectiveness of MSS
Table 7 reveals that the most effective of the MSS services offered the respondents included exclusive breast feeding on infant growth condition ( = 1.29), health talk on nutrition education and stress management ( = 1.21), positive and prompt response of SBAs toward respondents ( = 1.14) and child delivery service ( = 1.10). The least effective of the MSS services to the respondents were management of pregnancy complication cases ( = 0.19), ambulance service ( = 0.27) and availability of drugs at the MSS facility ( = 0.29). These indicate that the adoption of exclusive breastfeeding for infants, health talk given to respondents on nutrition and stress management and SBAs attention to their medical needs were the most effective maternal health services received. It can be inferred that the large advocacy of exclusive breast feeding from various programmes on safe maternal health, health talk on nutrition and stress management, likewise the readiness of skilled birth attendants to attend to pregnant and nursing mothers spurred respondents’ utilization of MSS. These findings are in line with Beaglehole and Dalpoz, [34] who found that that comfortable, secure, warm and proficient health service is crucial to better health practices and utilization.
| Table 7: Distribution of respondents by Effectiveness of MSS. | |||||
| Items | Highly Effective (%) | Effective (%) | Not Effective (%) | Rank | |
| Exclusive breast feeding on infant growth condition Health talk of nutrition education and stress management offered pregnant and child nursing women |
30.4 19.3 |
69.1 79.3 |
0.5 1.4 |
1.29 .21 |
1st 2nd |
| Positive and prompt response of SBAs toward pregnant women and nursing mothers | 12.6 | 85.5 | 1.9 | 1.14 | 3rd |
| Child delivery service Drugs prescribed by the SBAs for treatment of diseases and sicknesses Physical examination for blood pressure Advice on early initiation of breast feeding and lactation stimulating mechanisms to mothers who could not lactate early for the baby to suckle breast milk Laboratory service of scan for fetus development and possible disease diagnosis Cutting of umbilical cord and care of navel Blood test conducted to diagnose diseases and ascertain health status of patient Prevention of malaria and treatment of malaria |
10.6 7.2 6.3 8.2 7.7 7.7 5.8 7.8 |
89.4 90.3 92.8 88.9 88.4 87.9 91.8 85.0 |
0.0 2.5 1.0 2.9 3.9 4.3 2.4 7.2 |
1.10 1.07 1.05 1.05 1.04 1.03 1.02 1.01 |
4th 5th 6th 7th 8th 9th 10th 11th |
| Identification of conditions that require referral like anaemia and or bleeding vagina | 5.3 | 91.8 | 2.9 | 0.99 | 12th |
| Outreach service on vaccines as immunisation to children and sensitization on the gains of utilising MSS for child delivery | 7.2 | 65.7 | 27.1 | 0.92 | 13th |
| Provision of tetanus toxoid for mothers | 6.8 | 60.4 | 32.8 | 0.87 | 14th |
| Child vaccinations at the MSS facility Family planning service Screening and test before family planning Availability of drugs at the MSS facility anytime the SBAs prescribe medication for you |
6.3 40.1 5.8 6.3 |
57.0 50.7 48.3 16.9 |
36.7 9.2 45.9 76.8 |
0.84 0.80 0.60 0.29 |
15th 16th 17th 18th |
| Ambulance service | 5.3 | 15.9 | 78.7 | 0.27 | 19th |
| Management of pregnancy complication cases | 4.3 | 2.4 | 93.2 | 0.19 | 20th |
Respondents’ level of effectiveness of MSS
Table 8 reveals that the level of effectiveness of MSS was low in the study area, with 55.6% of women farmers having a mean score of less than 18. This implies that maternal health services available and offered to the respondents through MSS was not effective in its delivery of maternal health services. Thus, the poor effectiveness of MSS operations among the respondents could reduce their utilization of MSS. Ajilowo and Olujimi, [35] supported this finding that health services are more effective in the towns and cities than in the villages.
| Table 8: Distribution of respondents based on the levels of effectiveness of MSS. | |||||
| Levels of effectiveness of MSS | % | Minimum | Maximum | Mean | SD |
| Low High |
55.6 44.4 |
10.00 | 40.00 | 17.63 | 5.34 |
Test of hypotheses
Ho1: Relationship between respondents’ socioeconomic characteristics and utilization of MSS.
Table 9 reveals that significant relationship existed between the religion of women farmers and utilization of MSS (χ2 = 0.630, p < 0.05). This implies that religion did not contradict the use of MSS among women farmers, as it remains an environmental force in the society to propagate safe child birth ideas, beliefs, knowledge and ideal maternal ethical practices that could be used to propagate the utilization of MSS. Obasi, [36] supported this finding that the norm and practice of a society depends on systems of faith, custom and precepts guiding the existence of a people. Significant correlation existed between educational level of the women farmers and utilization of MSS (χ2 = 0.630, p > 0.05). This shows that the higher the women farmers were educated and enlightened the more they consciously seek and utilize MSS as the best option to safe maternal health. This result agrees with Etuk, et al. [37] who asserted that learning is instrumental and informative to knowledge search, likewise its usefulness among a group of people. Family size had significant correlation with MSS utilization (r = 0.523, p < 0.05). This implies that as the family size of the women farmers’ increases, there is a tendency for them to experience additional maternal risks from more family stress and different experiences of pregnancy and child birth, which could influence them to utilize MSS as a better alternative to other child delivery centres in their locality. This result negates the finding of Kebebe, et al. [38] that women with big family sizes seem not to deliver in orthodox health facilities.
| Table 9: Relationship between respondents’ socioeconomic characteristics and MSS Utilization. | ||||
| Variable | df | Chi-square value (χ2) | p - value | Decision |
| Religion | 3 | 2.040 | 0.001 | Significant |
| Educational level
Age Family size Monthly income |
4 | 12.85 r 0.079 0.117* 0.480* |
0.005
0.260 0.020 0.000 |
Significant
Not significant Significant Significant |
| Source: Field survey, 2019 * df means degree of freedom. | ||||
Monthly income had a significant correlation with MSS utilization among women farmers in the selected states (r = 0.480, p < 0.05). This shows that improved monthly income among the respondents strengthens their financial capability and opportunity to utilize MSS. Mansoor, et al. [39] supported this finding that utilization of modern health services among inhabitants of a community depends on its provision, efficacy, financial implication, people’s faith in the,
Ho2: Correlation between effectiveness and utilization of MSS.
The study reveals in table 10 that no significant correlation existed between effectiveness of MSS and the utilization of MSS in the study area (r = 0.605; p > 0.05). This implies that the lower the respondents’ expectations are met in terms of service delivery of MSS, the lower the tendency to utilize adequately. This might be that the evaluation of the respondents in terms of the services offered by MSS and its operations were not satisfactory enough and unconvincing for adequate utilization, despite producing actual result of safe pregnancy and child birth. This could be as a result of inadequacy in the quality of programme delivery, leading to non-significance of utilization among the respondents. The result agrees with Dairo and Owoyokun, [40] who found that women resident in areas with good infrastructure are prone to utilise orthodox medicine facilities actively than those resident in areas with poor infrastructural facilities.
| Table 10: Pearson Product Moment Correlation analysis of the correlation between effectiveness and Utilization of MSS. | |||||
| Independent Variable | SD | r | p | Decision | |
| Effectiveness | 17.63 | 5.34 | 0.605 | 0.107 | Not Significant |
| Field Survey, 2019. | |||||
Ho3: Significant differences in the level of MSS utilization among the respondents across states.
The study reveals in table 11 that a significant difference existed in the level of MSS utilization among the respondents across the three sampled states. This means that MSS utilization levels of the respondents vary from one state to another. This may not only be as a result of varying scales of their socioeconomic characteristics, but may also be due to varying levels of their maternal health information seeking behavior and effectiveness of MSS. This result is consistent with the finding of Ranjendra, et al. [41] that the predictors of women utilizing mother and child care health services are patterns of social relationships, pre-conceived notions, norms and values, mutual suspicion and disposition to skilled birth attendants, likewise proximity to orthodox health facilities and financial capability.
| Table 11: Analysis of variance of the differences in the levels of Utilization of MSS across states | ||||||
| Variable | Sum of squares | df | Mean square | F | p | |
| Utilization of MSS | Between groups | 1134.812 | 2 | 567.406 | 5.064* | 0.003 |
| Within groups | 22903.777 | 205 | 112.273 | |||
| Total | 24038.589 | 207 | ||||
The post hoc test, using Schaffer in table 12 further shows separation of means across the three states. It reveals that the level of utilization of MSS was higher and the same for respondents in Oyo State (49.2410 ± 11.39) and Ogun State (45.0806 ± 9.28), respectively while there was no significant difference between the level of MSS utilization in Ogun (45.0806 ± 9.28) and Ekiti (44.0000 ± 10.71). The similarities in the in MSS utilization levels by the respondents in Oyo and Ogun states and in Ogun and Oyo states, respectively may be connected with respondents’ maternal health information seeking behavior and effectiveness of MSS in the states.
| Table 12: Post hoc analysis of the separation of means for respondents’ level of MSS Utilization across the selected states. | |||
| Scheffe | |||
| States | N | Subset for alpha = 0.05 | |
| 1 | 2 | ||
| Ekiti | 62 | 44.0000 | |
| Ogun | 62 | 45.0806 | 45.0806 |
| Oyo | 83 | 49.2410 | |
| Sig. | 0.839 | 0.076 | |
The study concludes that women farmers are mainly in their reproductive ages of child bearing and active years of involvement in all aspects of agricultural activities, hence they expected to utilize MSS for safe maternal health and child care, sustainable for farm labour and farming occupation. Respondents are mainly small holder farmers participating in other livelihood activities, as secondary occupations for increased income, yet recorded low monthly income. Christianity was their predominant religion, Islam was also practiced among many and few were traditional worshippers, whose religious faith did not contradict the utilization of MSS. Many had a form of formal education but were subsumed to their husbands’ decision in utilization of MSS, with resultant effect of women farmers having little or no say on decision to utilize MSS for their maternal health. Also, sourcing of maternal health information was mainly through community health extension workers.
The study further concludes that respondents’ maternal health information seeking behavior on MSS was high. Utilization of MSS was moderate, which may be connected to low effectiveness of MSS. The most utilized MSS services were neonatal care, post natal care, skilled birth attendants, while the least utilized were ambulance service and referral service, owing to the premium women farmers placed on their infants’ survival and children as farm support. MSS utilization was concluded to be most utilized in Oyo and least utilized in Ekiti. The study concludes that the utilization of MSS is a function of the nexus of several factors, among which are accessibility to MSS, monthly income, sources of maternal health information, maternal health information seeking behavior and affordability of MSS.
Community health extension workers and Village Development Committee members should extend safe maternal health sensitization of MSS to husbands in rural communities for enhanced utilization of MSS by their wives, so as to mitigate against avoidable maternal death, improve child bearing women’s maternal health information seeking behavior towards MSS and strengthening of MSS utilization in the rural communities.
There is need for government at all levels, Non-Governmental Organizations (NGOs), civil societies and community leaders to harmoniously encourage all child bearing women in the rural areas to utilize MSS for their maternal health care. This will enhance more and adequate utilization of MSS facilities among rural women and prevent them from needless maternal death.
Government should provide Midwives Service Scheme facilities with laboratories, essential medical equipment and drugs, improve the basic social amenities in the farming communities like electricity and good rural road network to drive the functionality of the laboratories, and improve the effectiveness of Midwives Service Scheme, essential for effective utilization among child bearing women farmers.
Government should employ more skilled birth attendants to attend to the child bearing women utilizing MSS, in order to increase the skilled birth attendants’ ratio to the child bearing women. This will enhance more women farmers’ accessibility to SBAs and reduce their waiting time seeking the attention of SBAs on their maternal health needs.
Government should ensure that there is the provision of functional, standby and least expensive ambulance service at the MSS facilities for complicated and emergency cases that need quick referral to the general and tertiary hospitals in the urban areas, usually distant from the rural areas.
- Addai I. Determinants of use of maternal-child health services in rural Ghana. J Bio-Sociolog Sci. 2000; 32: 1-15. PubMed: https://pubmed.ncbi.nlm.nih.gov/10676056/
- Onasoga AO, Osaji TA, Alade OA, Egbuniwe MC. Awareness and Barriers to Utilization of Maternal Health Care Services Among Reproductive Women in Amassoma Community, Bayelsa State. Int J Nurs Midwifery. 2013; 6: 10-15.
- Conde-Agudelo A, Belizan JM, Lammers C. Maternal Prenatal Morbidity and ortality Associated with Adolescent Pregnancy in Latin America: Cross sectional study. Am J Obstet Gynecol. 2004; 192: 342-349. PubMed: https://pubmed.ncbi.nlm.nih.gov/15695970/
- Pitterson L. Making maternal mortality in Nigeria compelling enough. Media global voice of the global south. 2010. www.mediaglobal.com
- Dayaratna V, Winfrey W, Hardee K, Smith J, Mumford E, et al. Reproductive Health Interventions: Which Ones Work and What Do They Cost? Policy Project Occasional Paper 5. Futures Group International, Washington, D.C.2000.
- WHO. The World Health Report, 2004: Make Every Mother and Child Count, Geneva: WHO, 2004. www.who.int/healthpromotion/conferences/6gchp/en/
- Federal Ministry of Health. National Reproductive Health Policy and Strategy. Abuja, Nigeria. 2005.
- WHO. Maternal Mortality Fact Sheet. 2014. www.who.int/reproductivehealth
- Nnadi FN, Chikaire J, Atoma CN, Egwuonwu HA, Echetama JA. Ict for Agriculture Knowledge Management in Nigeria: Lessons and Strategies for Improvement. Sci J Agri Res Management. 2012; 7: 192-201.
- Aina LO. Library and information science text.Ibadan; Stirlin-Horden. 2004.
- Todaro MP. Economic development New York: Addison Wesley. 5th edition New York: Longman Group Ltd. 2000.
- Hill K, Thomas K, Abouzhr C, Walker N, Say L, et al. Estimates of maternal mortality worldwide between 1990 and 2005: An Assessment of Available Data. Lancet. 2007; 370: 1311-1319. PubMed: https://pubmed.ncbi.nlm.nih.gov/17933645/
- Nigeria Demographics Profile. 2011.
- Okonofua F, Lambo E, Okeibunor J, Agholor K. Advocacy for free maternal and child health care in Nigeria, results and outcomes. Health Policy. 2011; 99: 131-138. PubMed: https://pubmed.ncbi.nlm.nih.gov/20727612/
- Mojekwu JN, Ibekwe U. Maternal Mortality in Nigeria: Examination of Intervention Methods. Int J Humanities Soci Sci. 2012; 2: 4-9.
- Andersen RM Revisiting the behavioural model and access to medical care: Does it matter? J Health Sociol Behav. 1995; 36: 1-10. PubMed: https://pubmed.ncbi.nlm.nih.gov/7738325/
- National Population Commission. Nigeria Population by State. 2010. PubMed: http://www.population.gov.ng/index.php
- Vos T, Flaxman AD, Naghavi M, Lozano R, Michaud C, et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: Asystematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012; 380: 2163–2196. PubMed: https://pubmed.ncbi.nlm.nih.gov/23245607/
- Ayoade AR. Assessment of Women’s Involvement in Agricultural Production in Iddo Local Government Area: Implication for Agricultural and Rural Development in Oyo. Proceedings of the 21st Annual National Congress of the Nigerian Rural Sociological Association (NRSA). 2012; 27-34.
- Edna C, Mathew N, Adesope CON. Livelihood Diversity Strategies of Rural Women in Imo State Nigeria. Nigeria J Agricul Extension. 2007; 2: 117-123.
- Nwaobiala CU, Onumadu FN. Youth Participation in Cassava Production through Rural Extension. Proceedings of the 44th Annual Conference of Agricultural Society of Nigeria. 2010; 50-51.
- Nwaogwu DC, Echebiri RN, Eluu J. Determinants of Labour Supply and Output of Cassava Farmers in Ebonyi State, Nigeria. Proceedings of the 50th Annual Conference of Agricultural Society of Nigeria. 2016; 86-89.
- Adamu YM, Salihu HM. Barriers to use of antenatal and obstetric care services in rural Kano, Nigeria. J Obstetc Gynecol. 2002; 22: 600–603. PubMed: https://pubmed.ncbi.nlm.nih.gov/12554244/
- Hagedoorn J. Understanding the cross-level embeddedness of interfirm partnership formation. Academy of Management Review. 2006; 31: 670-680.
- Adekoya OA. The Patterns and Determinants of Agricultural Credit Use Among Farm Households in Oyo State, Nigeria. Asian Economic and Financial Review. 2014; 4: 1290-1297.
- Oludare CT, Jegede B. Baseline Assessment of Vulnerable Children and HIV Burden Alleviation in Ekiti State, Nigeria. Int J Sci Technol. 2012; 1: 1-14.
- Fasokun T, Katahoire A, Oduaran A. African Perspectives on Adult Learning: The Psychology of Adult Learning in Africa. University of Botswana, Botswana: Pearson Education. 2008.
- WHO. Factsheet, Maternal Mortality, Department of Making Pregnancy Safer. 2007.
- Babalola S, Fatusi A. Determinants of Use of Maternal Health Services in Nigeria Looking Beyond Individual and Household Factors. BMC Pregnancy Childbirth. 2009; 9: 43. PubMed: https://pubmed.ncbi.nlm.nih.gov/19754941/
- Anatasia JG, Marie GC. Effects of the physical accessibility of maternal health services on their use in rural Haiti. Population Studies. 2006; 60: 271-288. PubMed: https://pubmed.ncbi.nlm.nih.gov/17060054/
- Zhao QI, Kulane AS, Gao YI, Biao XU. Knowledge, attitude on maternal health care among rural to urban migrant women in Shangai, China BMC Women Health. 2009; 9: 5. PubMed: https://pubmed.ncbi.nlm.nih.gov/19298681/
- Okwa OO. Tropical parasitic diseases and women. Annals of African Medicine. 2007; 6: 157-163.
- Yahaya MK. Analysis of women's reproductisve health situation in Bida Emirate of Niger State, Nigeria. Africa J Reprod Health. 2004; 6: 50–64.
- Beaglehole R, Dalpoz MR. Public Health Workforce Challenges and Policy Issues. Human Resources for Health. 2003; 1: 478–491. PubMed: https://pubmed.ncbi.nlm.nih.gov/12904251/
- Ajilowo J, Olujimi B. Accessibility of the Rural Dwellers to Healthcare Facilities in Nigeria: The Owo experience. Pakistan J Soci Sci. 2007; 4: 44-55.
- Obasi OO. Understanding Society: An Introduction to Sociology. Treasure Books; Skill mark Media Ltd, Owerri, Nigeria. 2006.
- Etuk UR, Olatunji SO, Ekong I. Analysis of Health Needs on Self Medication Among Rural Farmers in Akwa-Ibom State, Nigeria. Nigerian J Agricul Food Environ. 2013; 9: 63-66.
- Kebebe E, Medhanit G, Dawit S, Kassahun N. Determinants of Community Based Maternal Health Care Service Utilization in South Omo Pastoral Areas of Ethiopia. 2012.
- Mansoor I, Hashimi NR, Mukhtaar F. Determinants and Pattern of Health Care Services Utilization in Postgraduate Students. 2009; 21: 100-105. PubMed: https://pubmed.ncbi.nlm.nih.gov/20929025/
- Dairo MD, Owoyokun KE. Factors affecting the utilization of antenatal care services in Ibadan, Nigeria. Benin J Postgrad Med. 2010; 12: 187-196.
- Ranjera K, Andy HL, Colin WB. Why women do not utilise maternity services in Nepal: WHO South East Asia. J Public Health. 2013; 2: 135-141. PubMed: https://pubmed.ncbi.nlm.nih.gov/28615588/
- Andersen RM. A behavioral Model of Families’ Use of Health Services. Research Series No. 25. Chicago, IL: Center for Health Administration Studies, University of Chicago. 1968.
- Connerton WC. Center for Health Outcomes and Policy Research. University of Pennsylvania School of Nursing. Contributions on “Midwifery” in Encyclopaedia Britannica. 2012. http://www.britannica.com/EBchecked/topic/381708/midwifery/302928/Midwifery-in-the-modern-e
- Food and Agricultural Organization. Towards sustainable food security: women and sustainable food security. 2010. www.fao.org
- Ideh O. Why Maternal Deaths Rise. The Nation. 2009.