More Information
Submitted: September 22, 2022 | Approved: October 12, 2022 | Published: October 13, 2022
How to cite this article: Bobokhojaev OI. Experience in optimizing the accessibility of services for tuberculosis in the Republic of Tajikistan. J Community Med Health Solut. 2022; 3: 064-068.
DOI: 10.29328/journal.jcmhs.1001022
Copyright License: © 2022 Bobokhojaev OI. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Tuberculosis; Access to services; Integrated approach; Intersectoral cooperation; Youth medical consultation centers
Experience in optimizing the accessibility of services for tuberculosis in the Republic of Tajikistan
Bobokhojaev OI*
National Institute of Meteorology, BP 156, 2035 Tunis-Carthage, Tunisia
*Address for Correspondence: Doctor of Medical Sciences, Professor, Head of the Department of Phthisiopulmonology, Avicenna Tajik State Medical University, Dushanbe, Tajikistan, Email: [email protected]
Actuality
Many researchers in their publications on tuberculosis (TB) in high-burden countries recommended the integrated work of different ministries and departments with the involvement of non-governmental public associations, volunteers, and activists, including former patients [1-8].
At the same time, a patient-oriented approach is prioritized in providing services to the population. Unfortunately, approaches to ensure the accessibility of young people to preventive services are not separately identified. Moreover, earlier studies among migrants point to insufficient coordination of activities of organizations in the field of health promotion, insufficient activity in the field of public information due to poor intersectoral approach, and insuffi-cient media activity [9-11].
Our previous studies indicate the existence of problems in the accessibility of the population of Tajikistan to medical, social, and TB services [12-15].
Purpose of the study
To study the impact of medical and social risk factors for TB among young people on access to medical services in the Republic of Tajikistan and develop ways to optimize it.
To understand the causes of the tense TB situation in the Republic of Tajikistan, a comprehensive study of social and medical factors influencing the development of TB in 390 healthy individuals and retrospective data from case histories of 200 TB patients was carried out. The age of the observed individuals in both groups ranged from 15 to 34 years. Men in both observed groups were 57.4% - 60.0%.
The first observation group, consisting of 390 healthy individuals, was recruited at the District Health Centers from among those undergoing a planned preventive medical examination, provided that specialists were concluded as healthy. The preventive examination included a study of a complete blood count, blood sugar, urinalysis, feces, chest x-ray and a consultation with a family doctor, endocrinologist, and TB specialist. Observation group 2, consisting of 200 TB patients, was recruited from among patients admitted for inpatient treatment at the National Center for Tuberculosis, Lung Diseases and Thoracic Surgery. The presence of concomitant diseases in TB patients was verified and stated in the medical history.
For a more detailed analysis of risk factors for TB in healthy individuals, we developed questionnaires that contain detailed information about TB awareness and stigma. The questionnaires were designed to identify the obstacles that the observed persons faced in relation to prevention, diagnosis, or treatment in general, and TB, if necessary. Informed consent was taken from all participants at the start of each survey. The goals and objectives of the study were clearly explained. The questionnaire consists of 50 questions and allows you to assess the socio-economic situation of the family and the conditions in which the respondents live. The questionnaire made it possible to assess the level of awareness of TB among healthy individuals. In-depth surveys of labor migrants were analyzed to identify issues such as lack of funds to pay for private consultations, the economic need to travel outside the country as a labor migrant, lack of knowledge about the curability of TB, or fear of social stigma and the possibility of becoming social outcasts. The data analysis used terms and concepts from the participants’ own phraseology in order to get to the heart of the matter. Residents of the Khatlon region, the Rasht valley, and the city of Dushanbe were equally selected for this study.
Data analysis
Upon completion, the questionnaires were coded and the data was prepared by entering them into the data entry program designed for the SPSS software.
An electronic version of the questionnaire was developed to simplify data analysis, which also made it possible to obtain a graphical display of data, with the minimum and maximum possible values. Statistical analysis of the study results was carried out using an IBM PC in the Microsoft Windows XP operating environment, using the Microsoft Excel 2007 application. The calculation of the sample mean error was carried out taking into account the deviation of the sample population - “n” from the general population - “p”, using Student’s coefficient - “t”. Statistically significant differences were taken into account when p was less than 0.05.
The minimum sample size for the study was determined using the EpiInfo version 6 Statcalc formula. The infinite population sample size is calculated as S = Z2 (P(1-P))/D2, where D is one-half the width of the desired sample confidence interval; Z is the percentile of a standardized normalized distribution defined by a specific confidence interval (CI); it is 1.95% for 95% CI. The adjustment factor for adjusting S to the final population and deriving a final sample size estimate was calculated using the formula “Sample size = S/(1+(S/population). In this study, 95% CI = Z = 1.96; p = 50%; D = 5%.
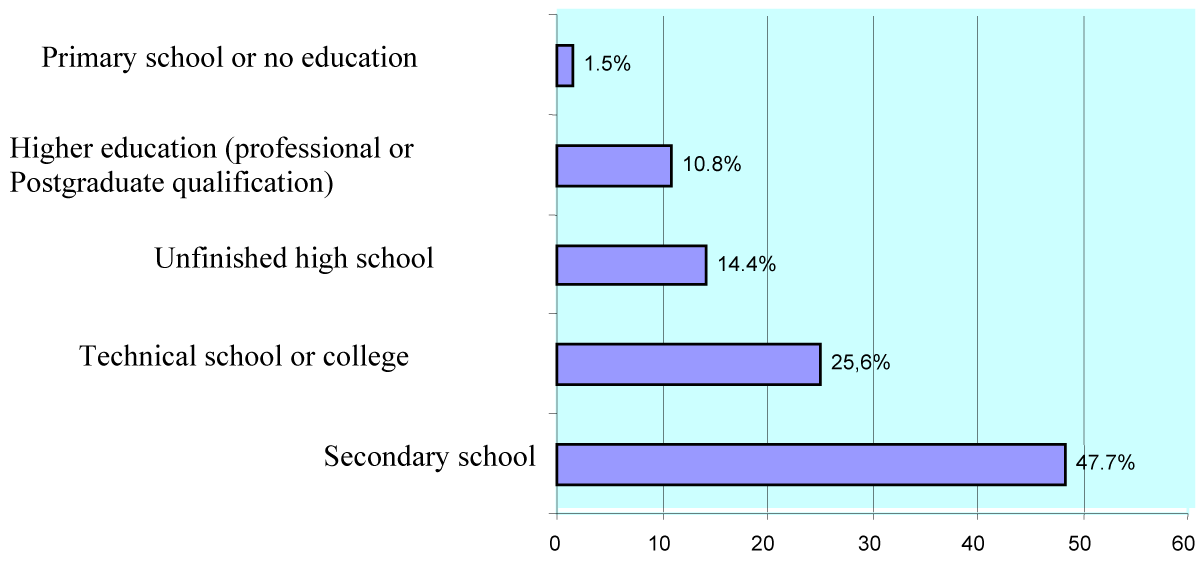
Socio-economic status of youth. A survey of healthy individuals revealed that only 10.8% of them had a higher education, 25.6% had specialized secondary education, and the rest had secondary and below secondary education (Figure 1).
Figure 1: The level of education of healthy individuals.
Most of the respondents lived in rural areas (76.9%). The standard of living of the surveyed healthy persons was assessed in accordance with the wages to cover the needs of the family. The survey showed that none of the respondents assessed their salary as adequate to cover the needs of the family. At the same time, the main needs of the family were called the weekly purchase of the necessary food products, the monthly purchase of the necessary non-food items, and the daily necessary transportation costs. And other services. Unfortunately, the consumer basket for young people in Tajikistan is not calculated and we are aware that the answers to these questions are very subjective. In this regard, among the respondents, the place of study or work was ranked as follows: 334 people, or 85.6% worked and the remaining 56 people or 14.4% studied. There was approximately the same number of men and women among working and students. Of the number of employees, 143 people, or 42.8% worked as some kind of specialists, and the other 191 people, or 51.2% - as auxiliary workers. Of the 191 people working as ancillary workers, 87 people (45.5%) were forced to leave the country as labor migrants. The main country of migration of respondents was the Russian Federation.
According to the length of stay of migration, 46 (52.9%) migrant workers stayed for more than one year, 24 (27.6%) - from 6 months to 1 year, and the remaining 17 (19.5%) - for less than 6 months.
The main reason for the return of migrants to Tajikistan was family reasons 41 people (47.1%). In 18 cases (20.7%) it was the loss of a job, 11 people (12.6%) reported health problems; 3 people (3.4%) were deported to Tajikistan, 8 people (9.2%) returned to Tajikistan blaming the financial crisis in Russia and 6 people (6.9%) returned for other reasons. Only 47 people. (54.0%) underwent a medical examination for employment.
The largest share of the surveyed migrants, i.e. 64 people (73.6%) worked in the construction industry. Others were employed in different fields, as shown in Table 1.
| Table 1: Type of employment of labor migrants. | ||
| Type of employment | Quantity | % |
| Construction | 64 | 73,6 |
| Trade | 11 | 12,6 |
| Transport | 5 | 5,7 |
| Industrial factory/factory | 2 | 2,3 |
| Shuttle trade | 2 | 2,3 |
| Agriculture | 2 | 2,3 |
| Catering | 1 | 1,2 |
| Total: | 87 | 100,0 |
Exposure to TB in persons who were in labor migration was determined according to their questionnaire: 58 people (66.7%) received good nutrition, 26 people (29.9%) ate twice a day, and 3 people (3.4%) - once a day.
A survey of housing conditions showed that only 11.5% of migrants had the opportunity to rent an apartment or a room, and the rest lived in crowded, poor living conditions (Table 2).
| Table 2: Housing conditions of labor migrants. | ||
| Housing | Quantity | % |
| Rented an apartment or a room | 10 | 11,5 |
| Sharing in a room: | ||
| up to 4 people | 44 | 50,6 |
| 4-8 people | 17 | 19,5 |
| more than 8 people | 12 | 13,8 |
| Workplace | 2 | 2,3 |
| Trailer (with 10 or more people) | 2 | 2,3 |
| Total: | 390 | 100,0 |
More than 20% of migrants, i.e. 18 people (20.7%) reported being in contact with a person with TB.
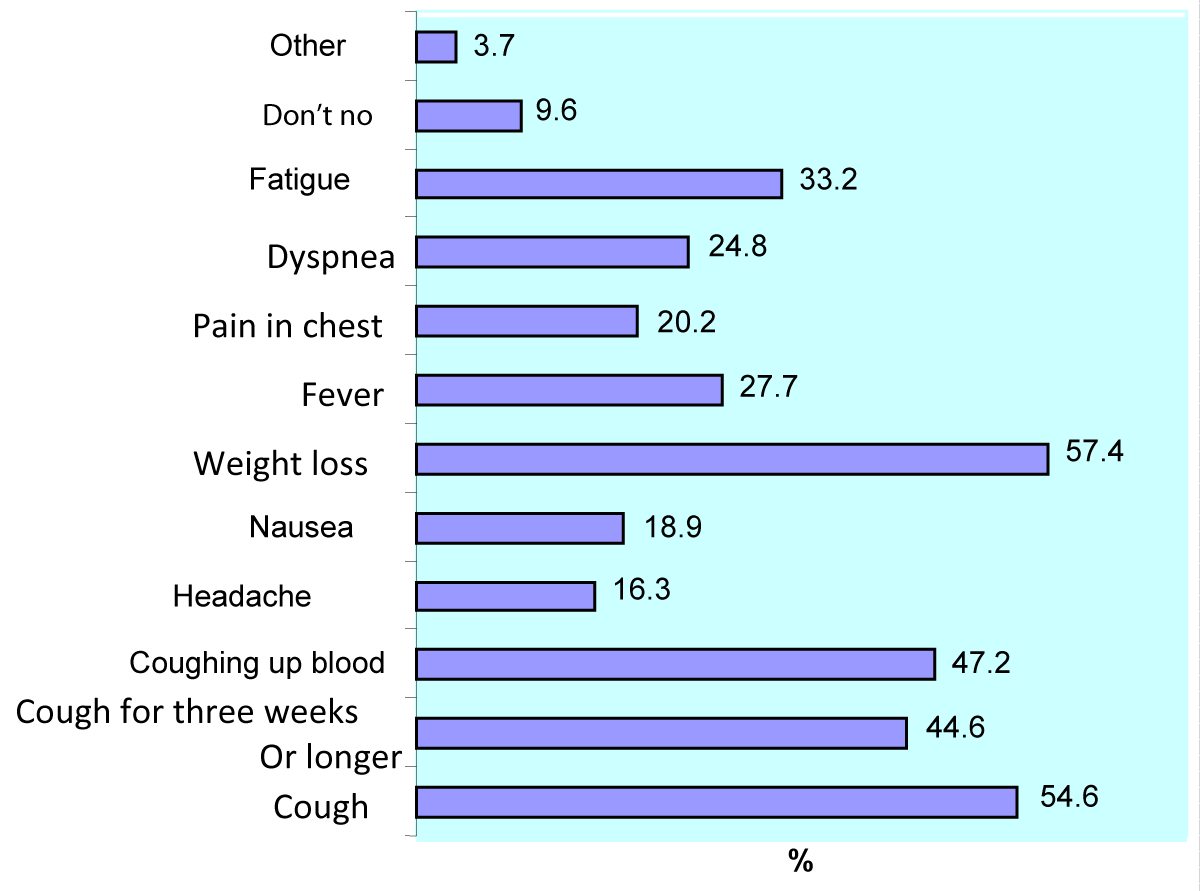
Level of youth awareness about TB. Of the 390 respondents, 213 people indicated cough as a manifestation of TB, and 174 people noted that the cough lasted for more than three weeks. 72 respondents noted both of the above features. Thus, a total of 315 people (80.7%) knew that the main manifestation of pulmonary TB is cough Figure 2.
Figure 2: Manifestations of TB, % (all symptoms are given).
The knowledge of the interviewees regarding the ways of transmission of TB was as follows (Table 3): 62.7% of people noted that TB can be transmitted when a TB patient coughs or sneezes. At the same time, 70% of respondents made mistakes pointing to the ways of TB transmission. 8.8% of the respondents noted that they do not know how TB is transmitted.
| Table 3: How can a person become infected with tuberculosis? (All mentioned answers are given). | ||
| Answers | Quantity | % |
| Sharing utensils | 273 | 70,1 |
| Eating from one plate | 259 | 66,4 |
| Airborne when a person coughs or sneezes | 244 | 62,7 |
| Through a handshake | 73 | 18,7 |
| Through touching objects in public places, such as doorknobs | 53 | 13,7 |
| Don't know | 34 | 8,8 |
| Sexually | 2 | 0,6 |
| Living in crowded housing | 1 | 0,2 |
According to the results of the survey, some population groups were classified as risk groups for developing TB - the poor (46.4%), the homeless (24%), alcoholics (24%), drug addicts (11.8%), HIV-infected (16.7%), prisoners in prisons (17.8%).
262 respondents (67.2%) rated TB as a serious disease, while 104 people (26.7%) underestimated the severity of TB.
324 respondents (83.1%) confirmed that TB is a curable disease (Table 4).
| Table 4: Can tuberculosis be cured?. | ||
| Answers | Quantity | % |
| Yes | 324 | 83,1 |
| Not | 54 | 13,8 |
| Some recover, some don't | 8 | 2,1 |
| People recover if treatment is started on time | 4 | 1,0 |
| Total: | 390 | 100 |
Level of stigma towards TB among young people. Most of the interviewed persons, i.e. 276 people (70.7%) would feel discouraged or hopeless if they were diagnosed with TB. Another common reaction was a feeling of fear, embarrassment, surprise, and shame (Table 3).
The majority of the interviewed persons – 320 persons (82.0%) would discuss their illness with a doctor or other healthcare professional. Only 5 people (1.2%) indicated that they would not discuss their illness with anyone.
182 respondents (46.8%) noted that TB patients should be treated in a friendly manner. 153 respondents (39.3%) emphasized that society should help TB patients and only 5 people (1.2%) were indifferent to the fate of TB patients and 3 (0.8%) did not know how to treat them.
Statistically significant differences were found in the total number of negative (227 people or 58.2%) and positive (163 people or 41.8%) results of the Mantoux test (p ˂ 0.01).
Of 200 TB patients with a history of the disease, comorbidities that preceded TB were detected in 68 patients: HIV infection in 11 patients, diabetes in 12 patients, COPD in 36 patients, hepatitis in 6 and peptic ulcer and duodenum - in 3 patients.
Our studies allow us to conclude that the main predictors of the development of TB among young people in Tajikistan are low social status and the associated high level of labor migration, poor living conditions, low level of awareness about the ways of transmission of tuberculosis, and the associated high level of stigma; high level of infection with Mycobacterium tuberculosis; the presence of concomitant diseases such as HIV infection, COPD and diabetes mellitus; moderate severity of malnutrition.
This analysis of the situation became the basis for the development of a system of measures aimed at counteracting the spread of socially determined diseases in Tajikistan, providing preventive, diagnostic, and treatment services to young people, including labor migrants and their families, in 3 ways:
➢ Integration of these services by ensuring intersectoral cooperation;
➢ Organization of Youth medical advisory centers at Health Centers, the main function of which is to provide the necessary information to young people and, if necessary, redirect them to specialists;
➢ Mandatory coverage of TB preventive treatment for persons with Mycobacterium tuberculosis infection, especially those with concomitant malnutrition and comorbidities such as HIV infection, COPD, or diabetes mellitus.
As a result, we have introduced in Tajikistan the method of an integral intersectoral approach to change the level of awareness, stigma, and discrimination. Within the framework of these positions, it is important to develop the medical-hygienic, socio-psychological direction, health promotion, and disease prevention of young people in the education system. This will be facilitated by the creation of a holistic system – the health school and a system of multi-level differentiated education of students, teachers, and parents, which allows optimizing the content, technologies, and organization of the pedagogical process to preserve physical, mental, and social health, personal development of each young person.
The tasks facing the state in the formation of a healthy lifestyle among young people, as well as the observance of the above principles of work, go far beyond the health sector and require the concerted efforts of all stakeholders. From these positions, in the field of forming a healthy lifestyle for school-age youth, it would be advisable to implement the following activities:
- Opening of the health school on the basis of the organization of secondary education and the inclusion of the subject “healthy lifestyle” and its conduct according to a single program approved by the Ministry of Education, Culture, Health and Social Protection of the Population, ensuring the training of teachers on this issue;
- Providing advisory and methodological assistance to healthcare and educational organizations in matters of protecting and promoting the health school, introducing, monitoring, and evaluating the implemen-tation of preventive programs (examination, screening, etc.), training specialists in the formation of a healthy lifestyle;
- Conducting information campaigns, extracurricular, and leisure activities among adolescents and young people to increase awareness, knowledge, and skills on the problems of formation of a healthy lifestyle;
- Development and strengthening of sports and leisure organizations, and youth health centers to provide comprehensive medical and preventive, socio-psychological assistance to adolescents and youth, in accordance with the provisions approved by the authorized bodies, support for NGOs implementing programs in the field of formation of a healthy lifestyle, the development of the volunteer movement;
- Assistance to all public schools, specialized and higher education institutions participating in the projects in organizing activities for cooperation and health promotion of adolescents and youth through the expansion of the State networks of “Health-Promoting Schools” and “Healthy Universities”.
Thus, the set of measures taken to optimize the accessibility of young people to preventive treatment and diagnostic services, including ensuring intersectoral cooperation, organizing a network of Youth Medical Consultative Centers at the Health Centers of each district of the country; Compulsory TB preventive treatment coverage of target individuals with Mycobacterium tuberculosis infection (Latent TB Infection), especially those with concomitant malnutrition and comorbidities such as HIV infection, COPD or diabetes mellitus, will help prevent of TB in healthy individuals and early diagnosis of Latent TB Infection and TB among persons with TB suspect.
The main obstacles to ensuring proper accessibility of young people to treatment and diagnostic services for TB are lack of information on services and, at the same time, fear of receiving information about the disease, geographical difficulties, psychological barriers, lack of social guarantees, and benefits, as well as payment for medical services. It is shown that the implementation of the method of an integral intersectoral approach to provide young people with specialized medical services with the involvement of state and public organizations, as well as the expansion of the network of youth medical advisory centers at Health Centers, ensure proper accessibility of young people to preventive and therapeutic and diagnostic services in general, including on TB, in particular.
- Creswell JH. Early and Increased Tuberculosis Case Detection: Implementation, Measurement, and Evaluation. PhD thesis. – New York: Faculty AMC-UvA, 2015; 213.
- Dangisso MH, Datiko DG, Lindtjørn B. Accessibility to tuberculosis control services and tuberculosis programme performance in southern Ethiopia. Glob Health Action. 2015 Nov 20;8:29443. doi: 10.3402/gha.v8.29443. PMID: 26593274; PMCID: PMC4655224.
- Kohler S, Asadov DA, Bründer A, Healy S, Khamraev AK, Sergeeva N, Tinnemann P. Ambulatory tuberculosis treatment in post-Semashko health care systems needs supportive financing mechanisms. Int J Tuberc Lung Dis. 2014 Dec;18(12):1390-5. doi: 10.5588/ijtld.14.0190. PMID: 25517802.
- MacPherson P, Houben RM, Glynn JR, Corbett EL, Kranzer K. Pre-treatment loss to follow-up in tuberculosis patients in low- and lower-middle-income countries and high-burden countries: a systematic review and meta-analysis. Bull World Health Organ. 2014 Feb 1;92(2):126-38. doi: 10.2471/BLT.13.124800. Epub 2013 Nov 22. PMID: 24623906; PMCID: PMC3949536.
- Raviglione M, Raviglione. Tuberculosis. In: Harrisons Principles of Internal Medicine. DI. Longo, et al. (Eds.) /. – USA: Hills Companies Inc. 2015; 1102-1122.
- Rubinowicz A, Bartlett G, MacGibbon B, Greenaway C, Ronald L, Munoz M, Menzies D. Evaluating the role of primary care physicians in the treatment of latent tuberculosis: a population study. Int J Tuberc Lung Dis. 2014 Dec;18(12):1449-54. doi: 10.5588/ijtld.14.0166. PMID: 25517810.
- Theron G, Peter J, Dowdy D, Langley I, Squire SB, Dheda K. Do high rates of empirical treatment undermine the potential effect of new diagnostic tests for tuberculosis in high-burden settings? Lancet Infect Dis. 2014 Jun;14(6):527-32. doi: 10.1016/S1473-3099(13)70360-8. Epub 2014 Jan 15. PMID: 24438820.
- Yassin MA, Datiko DG, Tulloch O, Markos P, Aschalew M, Shargie EB, Dangisso MH, Komatsu R, Sahu S, Blok L, Cuevas LE, Theobald S. Innovative community-based approaches doubled tuberculosis case notification and improve treatment outcome in Southern Ethiopia. PLoS One. 2013 May 27;8(5):e63174. doi: 10.1371/journal.pone.0063174. PMID: 23723975; PMCID: PMC3664633.
- Poletaev DV, Florinskaya YuF. Awareness of migrants about tuberculosis and HIV infection. IFRC&RC&RCC Research Report. - Moscow, 2015; 54.
- Dara M, Dara M. TB in Central Asia. Public Health Panorama. WHO. 2016; 2:10-14.
- John S, Gidado M, Dahiru T, Fanning A, Codlin AJ, Creswell J. Tuberculosis among nomads in Adamawa, Nigeria: outcomes from two years of active case finding. Int J Tuberc Lung Dis. 2015 Apr;19(4):463-8. doi: 10.5588/ijtld.14.0679. PMID: 25860003.
- Bobokhojaev OI, Khasanova S, Sirojiddinova UYu. Medico-social aspects of the development of tuberculosis among migrant workers of the Republic of Tajikistan. J Health of Tajikistan. 2011; 12-18.
- Bobokhojaev OI, Mahmudzoda IS, Gaibov AG. Risk factors for the development of tuberculosis in the Republic of Tajikistan. Bulletin of the Academy of Medical Sciences. Sciences of Tajikistan. 2016; 30-35.
- Bobokhojaev OI, Sirodzhidinova UYu, Dzhumaev RR, Mahmudzoda IS. On the issue of reactivation of the tuberculosis process. Bulletin of Avicenna. 2018; 20; 320-324.
- Sirojidinova UYu, Bobokhojaev OI, Dustmatova ZSh. Analysis of the tuberculosis situation in the Republic of Tajikistan. J Tuberculosis and Lung Diseases. Moscow, 2015; 32-36.