More Information
Submitted: January 11, 2024 | Approved: February 01, 2024 | Published: February 02, 2024
How to cite this article: Kumari R. Senile Cataract. J Community Med Health Solut. 2024; 5: 001-007.
DOI: 10.29328/journal.jcmhs.1001041
Copyright License: © 2024 Kumari R. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Lens; Cataract; Opacity; Age; Crystalline; Senile
Senile Cataract
Ragni Kumari*
Department of Optometry, Era University, Lucknow, India
*Address for Correspondence: Dr. Ragni Kumari, Department of Optometry, Era University, Lucknow, India, Email: [email protected]
Cataracts may be described as the opacity of crystalline lenses present in the eye. The translucent crystalline lens is a part of the human eye. It possesses all the physical characteristics of a biconvex lens. The eye’s lens performs similar functions to a camera’s lens. The lens directs light rays entering the eye to the retina’s sensitive layers. Any factor that increases the absorption of scattering of light by the lens reduces its transparency. The opacity of the lens or its capsule, whether developmental or acquired, is called a cataract. Cataracts vary in degree of density and site and assume various forms. Cataract is the leading cause of reversible visual impairment and blindness globally. There are several classifications of cataracts based on morphologic and/or etiologic criteria. However, in epidemiologic studies, the simplified system of three types based on localization of lens opacities is most commonly used: Nuclear cataract is the most common type, followed by cortical cataract and posterior subcapsular cataract. This most prevalent form of acquired cataract, also known as an “age-related cataract,” affects people of both sexes equally and typically develops after age 50. More than 90% of people experience senile cataracts by age 70. Although one eye is almost always afflicted before the other, the disorder is typically bilateral. In the available literature, there is no mention of any such drug that could reverse the opacity of the lens (cataract) once it occurred and make it clear and transparent again.
Only replacement of opaque lenses with artificial transparent Intraocular lens (IOL) is successful treatment of cataracts. This review focuses on senile cataracts and the best possible management of senile cataracts.
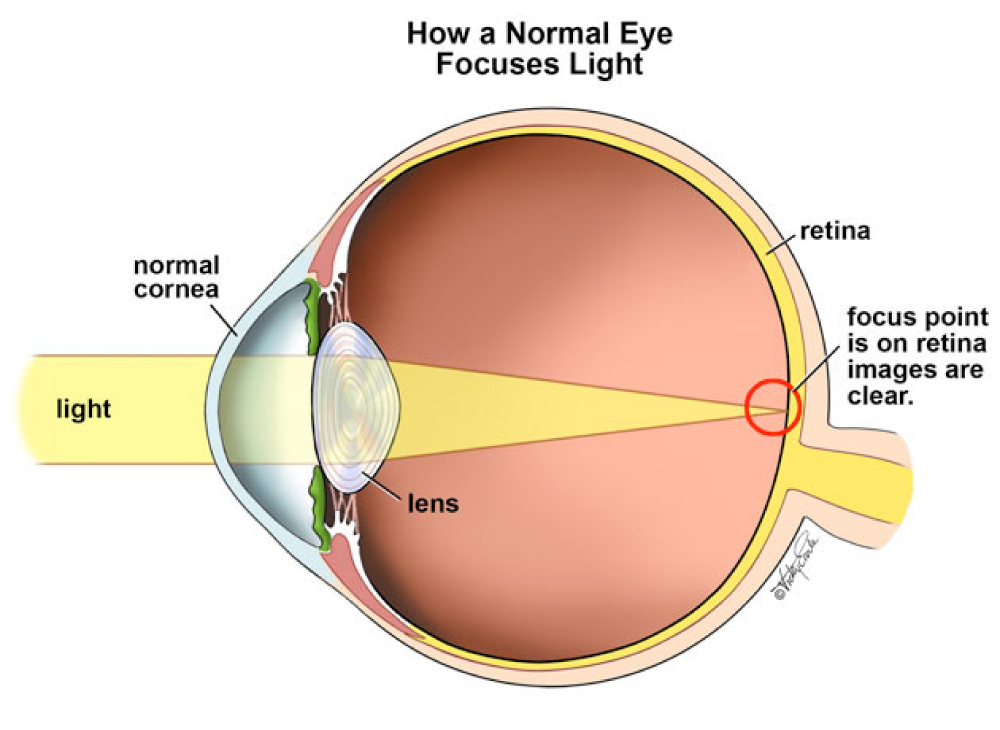
Cataracts may be described as the opacity of crystalline lenses present in the eye. The term cataract was introduced by Constantinus African (AD 1018). He translated the Arabic “suffusion” into Latin “Cataracta,” meaning “something poured underneath something,” the “waterfall.” The translucent crystalline lens is a part of the human eye. It possesses all the physical characteristics of a biconvex lens. The eye’s lens performs similar functions to a camera’s lens. The lens directs light rays entering the eye to the retina’s sensitive layers (Figure 1).
Figure 1: The normal eye focuses light on the retina. (Source: https://www.google.com/physics.stackexchange.com)
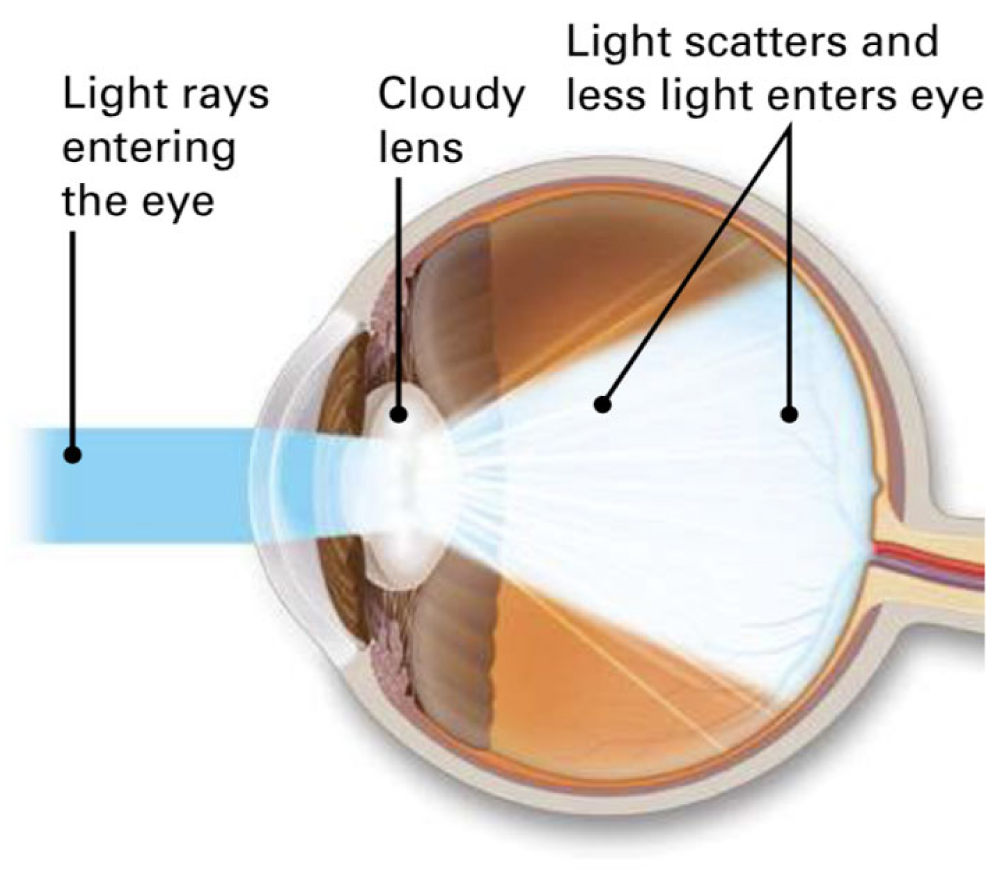
Any factor that increases the absorption of scattering of light by the lens reduces its transparency. The opacity of the lens or its capsule, whether developmental or acquired, is called a cataract (Figure 2). Cataracts vary in degree of density and site and assume various forms. Cataract is the leading cause of reversible visual impairment and blindness globally.
Figure 2: Light rays entering an eye with cataracts are not focused properly on the retina. (Source: https://www.strathfieldeyesurgery.com.au/eye-conditions/cataract/)
Age-related or senile cataracts are the primary cause of visual impairment in adults globally (65%). According to the accessibility of eye care services, their price, and the population’s level of eye care knowledge, there are significant differences in the causes between and within countries. In low- and middle-income countries, as opposed to high-income ones, a more significant percentage of vision impairment is related to cataracts. Glaucoma and age-related macular degeneration are more prevalent in nations with high incomes. Cataracts are the primary cause of severe vision impairment (80.7%), moderate visual impairment (70.2%), and blindness (66.2%) in India. Other significant factors contributing to blindness included corneal opacity (7.4%), complications from cataract surgery (7.2%), diseases of the posterior segment other than DR (Diabetic Retinopathy), and ARMD (Age-Related Macular Degeneration) (5.9%), and glaucoma (5.5%). Other than cataracts, various posterior segment illnesses, excluding DR and ARMD (3.4%), were the main contributors to significant vision impairment (8.3%). Maximum prevalence of blindness was seen in the 80+ age group (11.6%), followed by the 70-79 age group (4.1%), the 60-69 age group (1.6%), and the 50-59 age group (0.5%). Bijnor in Uttar Pradesh has the highest population suffering from blindness (3.67%) and visual impairment (21.82%) [1]. The aim of this review is to explore the prevalence, pathology, risk factors, and various management of senile cataracts.
Classification of cataracts
There are several classifications of cataracts based on morphologic and/or etiologic criteria. However, in epidemiologic studies, the simplified system of three types based on localization of lens opacities is most commonly used: Nuclear cataract is the most common type, followed by cortical cataract and posterior subcapsular cataract [2,3]. The World Health Organization has also proposed this classification [4]. Clinically cataracts may be classified based on morphology and underlying etiology.
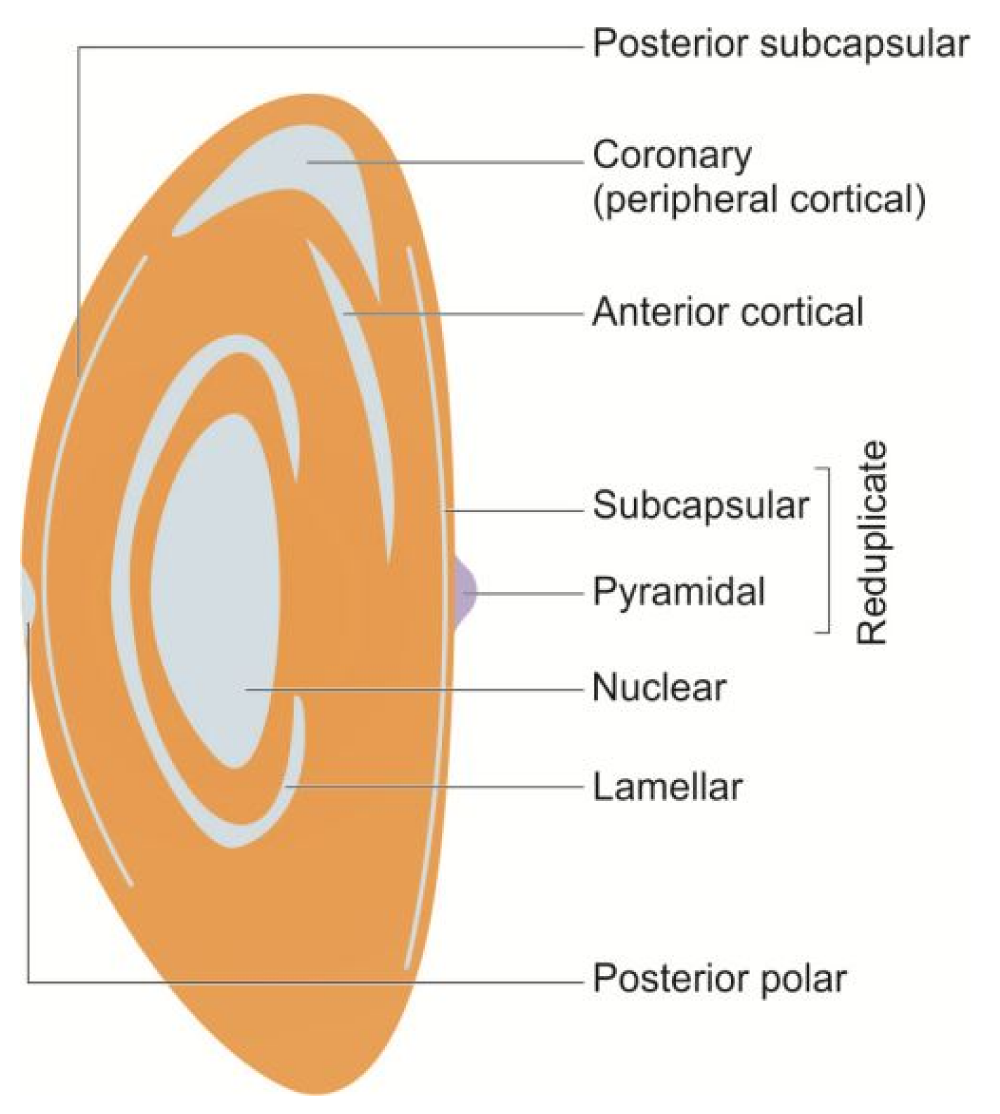
Morphologically cataracts can be divided into 6 parts: i. Capsular cataract. It involves the capsule and may be: Anterior capsular cataract and Posterior capsular cataract. ii. Subcapsular cataract. It involves the superficial part of the cortex (just below the capsule) and includes Anterior subcapsular cataracts and Posterior subcapsular cataracts. iii. Cortical cataract. It involves the major part of the cortex. iv. Supranuclear cataract. It involves only the deeper parts of the cortex (just outside the nucleus). v. Nuclear cataract. It involves the nucleus of the crystalline Lens. vi. Polar cataract. It involves the capsule and superficial part of the cortex in the polar region only and may be anterior polar cataract or Posterior polar cataract
Etiologically cataracts can be divided into Congenital or developmental cataracts and acquired. Congenital cataracts are further classified as Punctate, Polar, Sutural, Corraliform, Zonular and Coronary (Figure 3).
Figure 3: Diagrammatic representation of morphological types of cataracts. (Source: A. K. Khurana Comprehensive Ophthalmology, 2015 [15]).
Acquired cataracts are also further classified into, senile cataracts (age-related), complicated cataracts (ocular disease viz, uveitis, high Myopia, retinitis pigmentosa, glaucoma.), traumatic cataracts (in concussion or penetrating injuries of the eye), metabolic cataracts (in diabetes mellitus, tetany Wilson’s.), radiational cataracts (exposure to X-rays, Gamma rays, UV rays, IR rays, Microwaves, and LASER radiations.), dermatogenic cataracts (associated with the skin diseases such as atopic dermatitis) and toxic (in excessive or injudicious use of corticosteroid, miotics, chlorpromazine).
Senile cataract
This most prevalent form of acquired cataract, also known as an “age-related cataract,” affects people of both sexes equally and typically develops after age 50. More than 90% of people experience senile cataracts by age 70. Although one eye is almost always afflicted before the other, the disorder is typically bilateral.
Morphologically, the senile cataract occurs in two forms, the cortical (soft cataract) and the nuclear (hard cataract). Generally, the predominant form is cortical or cuneiform 70%, nuclear 25% and cupuliform or posterior or subcapsular 5%. It is common to find nuclear and cortical senile cataracts co-existing in the same eye. For this reason, it is difficult to accurately assess their relative frequency.
Pathophysiology of senile cataract
Specialized proteins (referred to as crystallins) are present in the lens, and their optical characteristics are based on the precise arrangement of their three-dimensional structure and hydration. Osmotic and ionic equilibrium is maintained throughout the lens by membrane protein channels. In contrast, the lens cytoskeleton, particularly the fiber cells of the nucleus, contributes to the distinctive form of the lens cells. High levels of reduced glutathione, known as the “mother of all antioxidants,” shield the protein-bound sulfhydryl (SH)-groups of crystallins against oxidation and cross-linking. The larger crystallins, which can absorb radiation energy (shortwave visible light, ultraviolet, and infrared radiation) over longer times without essentially changing their optical properties, give these materials high spatial and temporal stability (heat-shock proteins). This also provides a substantial protective function for the activity of various enzymes of carbohydrate metabolism (Hejtmancik, 2015). It is commonly acknowledged that oxidative stress plays a significant role in the onset of senile cataracts. The most common kind of cataract is found in cultured lens models and experimental animals. By producing peroxides and free radicals that obliterate all cell constituents, including proteins, lipids, and DNA, disturbances in the normal redox state of cells can have negative repercussions. A biological system’s capacity to quickly detoxify reactive intermediates or repair the harm they cause is at odds with the systemic manifestation of reactive oxygen species linked to oxidative stress that develops with aging. Age-related increases in oxidative lens processes lead to higher protein concentrations in opaque lenses. Proteins break down and clump together as a result, which damages fiber cell membranes. It has been scientifically proven that barriers in the aging eye prevent glutathione and other beneficial antioxidants from accessing the lens’ nucleus, leaving it vulnerable to oxidation (Pizzino 2017).
‘Cataract noxae’ can act and interact with one another as a result of aging to cause the development of different cataracts, many of which are linked to high protein-related light scattering and discolouration. Additionally, as the Lens ages, its metabolic efficiency decreases, increasing its susceptibility to harmful substances. Protein synthesis, transport, and membrane synthesis become difficult due to the glucose metabolic pathway’s very aerobic and poor energetic efficiency functioning due to aging. The epithelium and the tiny number of denucleated fiber cells, which still possess their metabolic arsenal, must also preserve the syncytial metabolic function of the denucleated fiber cells. Wedge or sectorial cataract formation results from a sharp inside-out metabolic gradient compounded by the lens acting like a whole new system and turning off damaged regions of fiber cells. The lens’s epithelial cells are stressed by radiation and light, which changes their genetic makeup. Due to their inability to extrude, faulty cells either undergo apoptosis or necrosis-based degradation or are relocated to the posterior capsular region, where they aid in developing posterior subcapsular cataracts [5].
The primary involvement of the AR pathway as the catalytic factor in developing diabetic cataracts has been the subject of extensive research. Aldose reductase, an enzyme, catalyzes the polyol pathway’s conversion of glucose to sorbitol, a process associated with the onset of diabetic cataracts. The enzyme sorbitol dehydrogenase converts sorbitol, which is generated at a high rate in the lens, into fructose. It has been demonstrated that the buildup of sorbitol inside cells causes osmotic alterations that cause hydropic lens fibers to deteriorate and develop into sugar cataracts. Furthermore, sorbitol’s polar nature limits its removal from cells by diffusion. A hyperosmotic action brought on by the increased sorbitol accumulation causes fluid to enter and cancel out the osmotic gradient. According to animal studies, the collapse and liquefaction of lens fibers caused by AR-mediated intracellular buildup of polyols result in lens opacities—the “Osmotic Hypothesis” of sugar cataract production results from these findings.
Additionally, nutritional and trace metal shortages, smoking, toxic chemicals like drug misuse, alcoholism, etc., and radiation (ultraviolet, electromagnetic waves, etc.) can cause oxidative stress and osmotic imbalance. It is causing the development of cataracts. However, it is obvious that the precise pathophysiology of the risk mentioned above factors needs to be understood [5].
Factors affecting age of onset, type and maturation of senile catara:
- Heredity. It plays a considerable role in the incidence, age of onset, and maturation of senile cataracts in different families.
- Ultraviolet irradiations. More exposure to UV irradiation from sunlight has been implicated in the early onset and maturation of senile cataracts in many epidemiological studies.
- Dietary factors. A diet deficient in certain proteins, amino acids, vitamins (riboflavin, vitamin E, vitamin C), and essential elements has also been blamed for the early onset and maturation of senile cataracts.
- Dehydration crisis. An association with a prior episode of severe dehydration crisis (due to diarrhea, cholera, etc.) and age of onset and maturation of cataract is also suggested.
- Smoking causes accumulation of pigmented molecules—3 hydroxykynurenine and chromophores- leading to yellowing—cyanates in smoke cause carbamylation and protein denaturation. Smoking has also been reported to have some effect on the age of onset of senile cataracts.
Role of UV radiation in cataract development
The two main mechanisms for introducing cataracts by ocular UV light exposure are oxidative stress and the resulting inflammation [6] and photooxidation, which may involve photosensitizers [7]. These may be endogenous substances, such as metabolites of inert tryptophan that become enzymatically altered with age [8], UV-absorbing advanced glycation end products [9], or exogenous photosensitizers, such as phototoxic drugs [10]. All these mechanisms generate reactive oxygen species (singlet oxygen and/or superoxide) that oxidize lens proteins, gradually forming opacities that eventually develop into cataracts [7]. The most diffuse source of human UV exposure is solar radiation, including the entire spectrum of UV bands. However, UV-C and much of UV-B are absorbed in the atmosphere, mainly by ozone: current ozone depletion increases UV-B exposure. Other optical regions of the solar spectrum also have the potential to cause chronic photochemical lens damage, e.g., blue light, especially in the presence of phototoxic drugs, but their role in cataract pathogenesis is less clear [11,12].
Clinical features of senile cataract
Clinical feature of cataracts varies according to the stage of development of cataracts.
- Stage of lamellar separation: In this stage, the patients experience Blurring of vision, frequent change of glasses due to rapid change in the refractive index of the lens, and the painless, progressive, gradual diminution of vision. It can be diagnosed on slit lamp examination (cannot be seen by the naked eye).
- Incipient stage: In this stage the patients experience, Polyopia and see colored halos. On an ophthalmoscopy lens, opacities appear as black spots against a red background.
- Intumescent stage: In this stage, the patients experience glare in sunlight and progressively diminish vision. On examination, the iris shadow can be seen on the lens.
- Immature cataract: On reaching this stage the patients experience reduced night vision in cortical cataracts, reduced day vision in cortical cataracts, and second sight or myopic shift in nuclear cataracts. Signs include, the iris's shadow being present on the lens, and opacity in the lens appearing as black spots against a red background on ophthalmoscopy.
- Mature cataract: In mature cataracts visual acuity is noticeably reduced (maybe reduced to the extent of PL positive only). Signs include: iris's shadow is absent, no fundal glow was seen on ophthalmoscopy, in cortical cataract lens appears, pearly white, and in nuclear cataract lens appears colored.
- Hypermature cortical cataract (Morgagnion cataract): The lens cortex gets liquified, and the nucleus settles down in the capsular bag.
Management of senile cataract
In the available literature, there is no mention of any such drug that could reverse the opacity of the lens (cataract) once it occurred and make it clear and transparent again.
i. Prophylaxis of senile cataract: Age-related cataract is a multi-factorial disease, and genetic and environmental factors contribute to cataract development [13], including nutrition. Smoking, exposure to ultraviolet rays, and diabetes are known risk factors for developing cataracts. Cigarette smoking is linked to increased risk factors for nuclear sclerosis. A cortical cataract is common in people who work in open farms and fields and are exposed to ultraviolet light. Preventive strategies include avoiding smoking, abstinence from alcohol, judicious use of steroids, use of protective glasses to shield against sunlight, and strict glycemic control in diabetic patients. Epidemiological research suggests that the risk of cataracts can be diminished by adhering to diets that contain high levels of vitamin C, lutein, zeaxanthin, B vitamins, omega-3 fatty acids, and multivitamins and avoiding frequent and large intakes of simple carbohydrates. In the Age-Related Eye Disease Study, intake of a multivitamin supplement was moderately protective against the development of cataracts [14]. The role of aspirin and antioxidants in delaying the progress of cataractogenesis remains inconclusive. Because cataract is a degenerative disease mainly caused by aging, overall recommended prevention methods are unsatisfactory.
ii. Non-surgical measures
1. Measures to delay progression: Even though there is no established medical treatment for cataracts, many commercially available preparations containing iodide salts of calcium and potassium, cineraria maritima, etc., are being prescribed in abundance in the early stages of cataracts (especially in senile cataracts) in a bid to delay its progression. However, to date, conclusive results about their role have yet to be available. The role of vitamin E and aspirin in delaying the process of cataractogenesis is also mentioned.
2. Measures to improve vision in the presence of incipient and immature cataracts:
These include:- Refraction, which often changes rapidly, should be corrected at frequent intervals.
- Arrangement of illumination. Patients with free peripheral opacities (a pupillary area) may be instructed to use brilliant illumination. Conversely, a dull light placed beside and slightly behind the patient's head in central opacities will give the best result.
- The use of dark goggles in patients with central opacities is of great value and comfort when worn outdoors.
3. Mydriatics: Patients with small axial cataracts frequently may benefit from pupillary dilatation. This allows the clear paraxial Lens to participate in light transmission, image formation, and focus. Mydriatics such as 5% phenylephrine or 1% tropicamide; 1 drop b.i.d. in the affected eye may clarify the vision.
iii. Surgical measure
It is re-emphasized that presently there is no medical treatment for cataracts. The only effective treatment of cataracts is surgical removal. The surgical indications for when to take up cataract surgery are needed:
- Visual development: This is by far the most typical symptom. Depending on the individual's visual needs, different people may need surgery at different times for vision improvement. Therefore, a person should have cataract surgery when the visual impairment significantly interferes with leading a normal life.
- Medical indications: Sometimes patients may be comfortable from the visual point (due to useful vision from the other eye or otherwise) but may be advised cataract surgery due to medical grounds such as Lens induced glaucoma, Phacoanaphylactic endophthalmitis and Retinal diseases like diabetic retinopathy or retinal detachment, treatment of which is being hampered by the presence of lens opacities.
- Cosmetic indication: Sometimes patients with mature cataracts may insist on cataract extraction (even with no hope of getting useful vision) to obtain a black pupil
Types of surgical techniques
The introduction of fine needles, suture material, and an operating microscope has made cataract surgery very safe.
i. Intracapsular cataract extraction (ICCE): In this technique, the entire cataractous Lens, along with the intact capsule, is removed. Therefore, this approach requires weak and degenerated zonules. This means that this procedure cannot be used on younger individuals with significant zonules. Between the ages of 40 and 50, ICCE can be carried out utilizing alpha chymotrypsin to dissolve the zonules. Most of the time, this enzyme is not required after the age of 50. ICCE can be performed between 40-50 years of age using alpha chymotrypsin (which will dissolve the zonules). Beyond 50 years of age, usually, there is no need for this enzyme.
Indications: ICCE has stood the test of time and has been widely employed for about 50 years all over the world. Now (for the last 25 years), it has been almost entirely replaced by planned extracapsular technique. Currently, the only indications of ICCE are markedly subluxated and dislocated Lenses.
ii. Extracapsular cataract extraction (ECCE): This technique removes a major portion of the anterior capsule with epithelium, nucleus, and cortex, leaving behind an intact posterior capsule. Phacoemulsification and small incision cataract surgery have improved the quality of vision and reduced the convalescence time of patients. Currently, planned ECCE with IOL implantation is the most preferred surgery.
Indications: The extracapsular cataract extraction technique is the surgery of choice for almost all types of adulthood and childhood cataracts unless contraindicated. Contraindications. The only absolute contraindication for ECCE is a markedly subluxated or dislocated Lens.
Merits and demerits of various surgical techniques
I. Merits of Extracapsular Cataract Extraction (ECCE) over Intracapsular Cataract Extraction (ICCE):
- ECCE is a universal operation that can be performed at all ages, except when zonules are not intact, whereas ICCE cannot be performed below 40.
- Posterior chamber IOL can be implanted after ECCE, while it cannot be implanted after ICCE. 3. Postoperative vitreous-related problems (such as herniation in the anterior chamber, pupillary block, and vitreous touch syndrome) associated with ICCE are not seen after ECCE.
- Incidences of postoperative complications such as endophthalmitis, cystoid macular edema, and retinal detachment are much less after ECCE than after ICCE.
- Postoperative astigmatism is less, as the incision is smaller.
ii. Merits of Small Incision Cataract Surgery (SICS) over Conventional Extracapsular Cataract Extraction (ECCE)
- Small size incision.
- No surgery is required.
- Close chamber surgery with no or least risk of vitreous prolapse, operative hard eye, and expulsive choroidal hemorrhage.
- Least postoperative astigmatism.
- No postoperative suture-related problems like irritation and suture abscess etc.
- No postoperative wound-related problems such as wound leak, shallowing of the anterior chamber, and iris prolapse.
- No need for suture removal, during which infection may occur.
iii. Merits of manual Small Incision Cataract Surgery (SICS) over phacoemulsification
- Universal applicability, i.e., all types of cataracts, including hard cataracts (grade IV and V), can be operated by this technique.
- Learning curve. This procedure is much easier to learn as compared to phacoemulsification.
- Not machine-dependent. The biggest advantage of manual SICS is that it is not machine-dependent and thus can be practiced anywhere.
- Less surgical complications. Dis disastrous complications like nuclear drop into the vitreous cavity are much less than the phacoemulsification technique.
- Operating time in manual SICS is less than phacoemulsification, especially in hard cataracts. Therefore, it is ideal for mass surgery.
- Cost-effective. With manual SICS, the expenses are vastly reduced as compared to the considerable expenses of acquiring and maintaining a phaco machine.
- Conjunctival congestion persists for 5-7 days at the site of the conjunctival flap.
- Mild tenderness sometimes may be present owing to scleral incision.
- Postoperative hyphaema may be noted sometimes.
- Surgical-induced astigmatism is more common as the incision in SICS is large (about 6 mm) as compared to phacoemulsification (about 3.2 mm).
v. Merits of phacoemulsification over manual Small Incision Cataract Surgery (SICS)
- Topical anesthesia may be sufficient for phacoemulsification in expert hands.
- Postoperative congestion is minimal after phacoemulsification, as surgery is usually performed through a clear corneal incision.
- Small incision. The chief advantage of phacoemulsification over manual SICS is that it can be performed through a smaller (3.2 mm) incision.
- Less corneal complications. Phacoemulsification can be performed in the posterior chamber without prolapsing the nucleus into the anterior chamber, thereby minimizing the risk of corneal complications.
- Visual rehabilitation is comparatively quicker in phacoemulsification as compared to manual SICS.
- Postoperative astigmatism is comparatively less when foldable IOLs are implanted through a smaller incision (3.2 mm).
Limitations of phacoemulsification
- The learning curve for phacoemulsification is more painful for surgeons and patients.
- Complications encountered during phacoemulsification, like nuclear drop, are unforgiving.
- Machine dependent. This procedure is solely machine-dependent, and in the event of an unfortunate machine failure in the middle of surgery, one must shift to conventional ECCE.
- High cost. The cost of this technique is very high because of the expensive machines, accessories, and maintenance.
- It is very difficult to deal with hard cataracts (grade IV and V) with this technique, and there is a high risk of serious corneal complications due to more use of phaco energy in such cases.
The pathophysiological position of the oxidant-antioxidant balancing systems in the lens and cataract blindness is justified. Oxidative damage on the lens induces membrane damage, metal accumulation, protein modification and accumulation, inflammation, lenticular apoptosis, etc. and all these alter the refractive properties of the lens resulting in opacity and cataracts. Although modern surgical procedures are available for cataract treatment, they have their own limitations and complications and natural product-based nutritional therapy is a newly emerging cost-effective area in the field of vision research for cataract management by way of precautionary protection.
- National Programme for Control of Blindness &Visual Impairment, Directorate General of Health Services, MHFW, New Delhi. 2019.
- Hall AB, Thompson JR, Deane JS, Rosenthal AR. LOCS III versus the Oxford Clinical Cataract Classification and Grading System for the assessment of nuclear, cortical and posterior subcapsular cataract. Ophthalmic Epidemiol. 1997 Dec;4(4):179-94. doi: 10.3109/09286589709059192. PMID: 9500153.
- Thylefors B. A global initiative for the elimination of avoidable blindness. Indian J Ophthalmol. 1998 Sep;46(3):129-30. PMID: 10085623.
- Thylefors B, Chylack LT Jr, Konyama K, Sasaki K, Sperduto R, Taylor HR, West S; WHO Cataract Grading Group. A simplified cataract grading system. Ophthalmic Epidemiol. 2002 Apr;9(2):83-95. doi: 10.1076/opep.9.2.83.1523. PMID: 11821974.
- Michael R, Bron AJ. The ageing lens and cataract: a model of normal and pathological ageing. Philos Trans R Soc Lond B Biol Sci. 2017; 366: 1278–1292.
- Osnes-Ringen O, Azqueta AO, Moe MC, Zetterström C, Røger M, Nicolaissen B, Collins AR. DNA amage in lens epithelium of cataract patients in vivo and ex vivo. Acta Ophthalmologica. 2013; 91(7): 652–656. doi:10.1111/j.1755-3768.2012.02500.x
- Roberts JE. Ultraviolet radiation as a risk factor for cataract and macular degeneration. Eye Contact Lens. 2011 Jul;37(4):246-9. doi: 10.1097/ICL.0b013e31821cbcc9. PMID: 21617534.
- Balasubramanian D. Ultraviolet radiation and cataract. J Ocul Pharmacol Ther. 2000 Jun;16(3):285-97. doi: 10.1089/jop.2000.16.285. PMID: 10872925.
- Ortwerth BJ, Prabhakaram M, Nagaraj RH, Linetsky M. The relative UV sensitizer activity of purified advanced glycation endproducts. Photochem Photobiol. 1997 Apr;65(4):666-72. doi: 10.1111/j.1751-1097.1997.tb01909.x. PMID: 9114742.
- Roberts J. Screening dyes, drugs, and dietary supplements for ocular phototoxicity. In Photostability of Drugs and Drug Formulations, Second Edition. 2004; 235–254. doi:10.1201/9781420023596.ch11
- Taylor HR, West S, Muñoz B, Rosenthal FS, Bressler SB, Bressler NM. The long-term effects of visible light on the eye. Arch Ophthalmol. 1992 Jan;110(1):99-104. doi: 10.1001/archopht.1992.01080130101035. PMID: 1731731.
- Sliney DH. Intraocular and crystalline lens protection from ultraviolet damage. Eye Contact Lens. 2011 Jul;37(4):250-8. doi: 10.1097/ICL.0b013e31822126d4. PMID: 21670691.
- Shiels A, Bennett TM, Knopf HL, Maraini G, Li A, Jiao X, Hejtmancik JF. The EPHA2 gene is associated with cataracts linked to chromosome 1p. Mol Vis. 2008;14:2042-55. Epub 2008 Nov 12. PMID: 19005574; PMCID: PMC2582197.
- Age-Related Eye Disease Studies (AREDS/AREDS2) | National Eye Institute. 2023. https://www.nei.nih.gov/research/clinical-trials/age-related-eye-disease-studies-aredsareds2
- Khurana A. Comprehensive Ophthalmology. Jaypee Brothers Medical Publishers (P) Ltd. eBooks. 2015. https://doi.org/10.5005/jp/books/12532