More Information
Submitted: January 10, 2023 | Approved: April 12, 2024 | Published: April 15, 2024
How to cite this article: Zimamu LY, Adal GM, Wubet GM, Alemnew D. Hypo-glycaemia and Associated Factors among Type 1 Diabetes Mellitus Patients Attending the Outpatient Clinics of Debre-tabor Compressive and Specialized Hospital, South Gondar Zone, North West Ethiopia: A Cross-sectional Study. J Community Med Health Solut. 2024; 5: 031-043.
DOI: 10.29328/journal.jcmhs.1001045
Copyright License: © 2024 Zimamu LY, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Hypoglycemia; Diabetes mellitus; Debre-Tabor; Ethiopia
Acronyms and abbreviations: AOR: Adjusted Odds Ratio; BSc: Bachelor of Science; CI: Confidence Interval; DC: Data Collectors; DM: Diabetes Mellitus; ETB: Ethiopian Birr; GP: General Practitioner; DTCSH: Debra-Tabor Comprehensive and Specialized Hospital; HbA1c: Hemoglobin A1c; KAP: Knowledge Attitude and Practice; MOH: Ministry of Health; OHA: Oral Hypoglycemic Agent; OPD: Out Patient Department; RHB: Regional Health Bureau; SPSS: Statistical Package for Social Science; DTU: Debre - Tabor University; OR: Odds Ratio; PI: Principal Investigator
Hypo-glycaemia and Associated Factors among Type 1 Diabetes Mellitus Patients Attending the Outpatient Clinics of Debre-tabor Compressive and Specialized Hospital, South Gondar Zone, North West Ethiopia: A Cross-sectional Study
Libsuye Yalgaw Zimamu1*, Gashaw Mekete Adal1, Gashaw Mehiret Wubet2 and Dessie Alemnew3
1Debre Tabor, College of Health Science, Department of Health informatics, Debre Tabor, Ethiopia
2Debre Tabor University, College of Health Science, School of Medicine, Debre Tabor, Ethiopia
3Debark University, College of Health Science, School of Medicine, Debark, Ethiopia
*Address for Correspondence: Libsuye Yalgaw Zimamu, BSc, Debre Tabor, College of Health Science, Department of Health informatics, Debre Tabor, Ethiopia, Email: [email protected]
Introduction: Hypoglycemia affects patient safety and glycemic control during insulin treatment of both type 1 (T1DM) and type 2 diabetes mellitus (T2DM). It is still a major clinical problem in the treatment of type 1 diabetes that impairs metabolic control. This study aimed to assess hypoglycemia and associated factors among type 1 diabetes mellitus patients attending the outpatient clinics of Debra–Tabor Comprehensive and Specialized Hospital, in 2021.
Method: institutional-based cross-sectional study design was conducted among 204 selected type I DM, from June 1/2021 to August 30/2021. The study participants were selected by systematic sampling method from monthly follow-up lists and lists of registration. Data were cleaned and entered into Epi Data and then exported into SPSS version 20 for analysis. Data were presented with texts, graphs, diagrams, and tables but an analytic form of findings will be presented by text form of the odds ratio. Bivariable and multivariable binary logistic regression models were fitted to identify factors associated with hypoglycemia p – value < 0.05 was considered statistically significant and reported as a 95% confidence interval (CI).
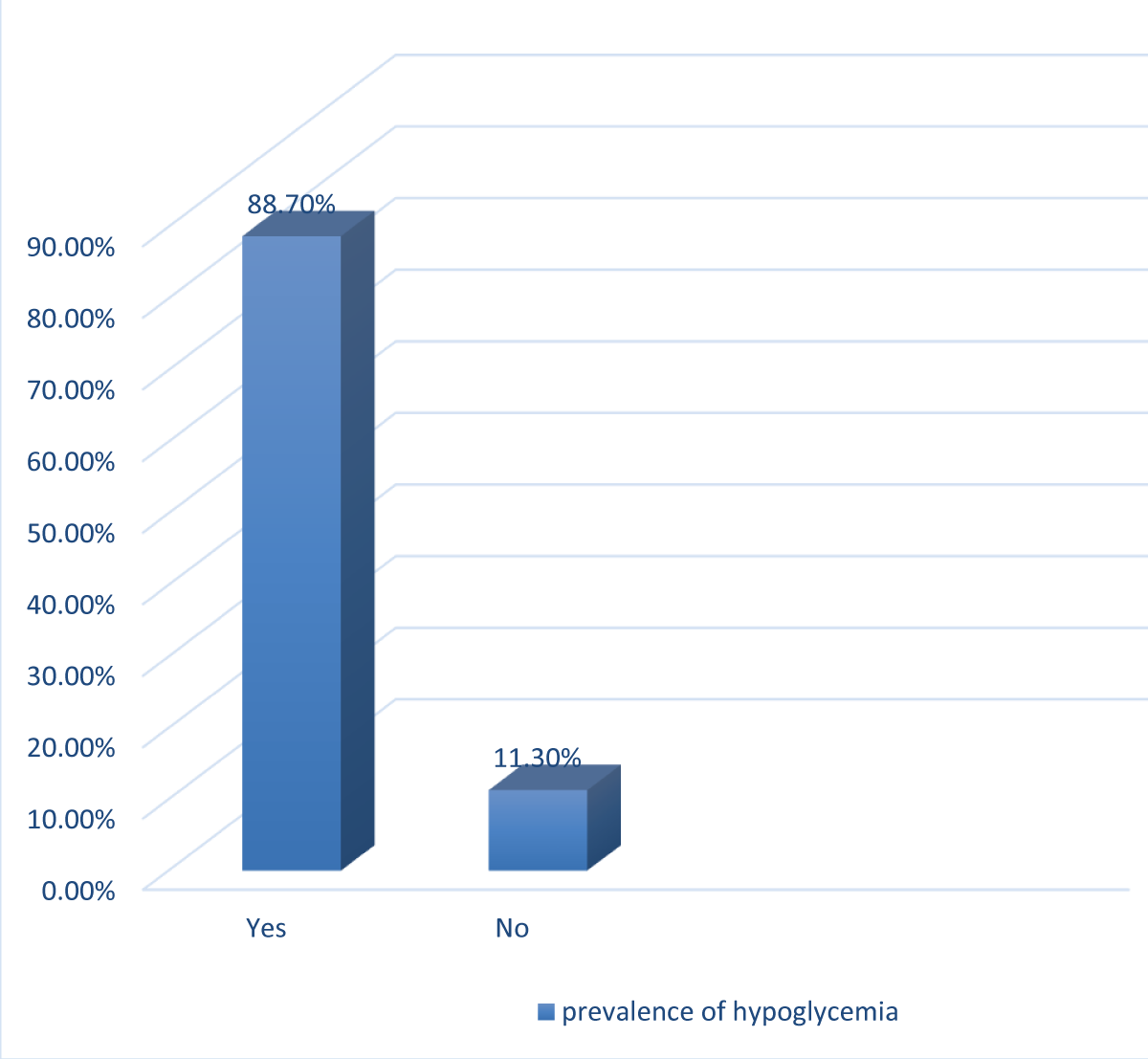
Results: A total of 204 participants participated with a response rate of 100% and prevalence of self-reported hypoglycemia was 88.7% (95%, CI: 83.8-92.6) and the prevalence of hypoglycemia was significantly associated with occupation [AOR: 4.01 (95% CI:1.86-9.35)], higher educational status [AOR: 2.13 (95% CI:1.92-13.15)], diabetic duration < 1 [AOR: 3.80 (95% CI:1.32-9.28)], poor knowledge [AOR: 4.91 (95% CI:1.09-11.06)] and favorable attitude [AOR: 5.86(1.10-6.07)]. The current study revealed that the knowledge, attitude, and practice of respondents were 81.9% (95%, CI, 76-86.8), 73% (95% CI, 66.7-78.9), and 91.2% (95% CI, 86.8-94.6) respectively
Conclusion and recommendation: Hypoglycemia was highly prevalent among diabetic patients treated at Debra-Tabor Comprehensive and Specialized Referral Hospital. To reduce the higher prevalence of hypoglycemia the health professionals working in the hospital had better provide appropriate patient advice about, BGL monitoring, medication adherence, self-injection as well as oral hypoglycemic agent administrations.
Background
Hypoglycemia is defined as when the blood glucose level of the adult drops < 70 mg/dl [1-3]. Hypoglycemia is also one of the short-term complications of increased longevity, and improved health outcomes with tight glycemic control alarming for a hemoglobin A1c (HbA1c) concentration below 6.5% - 7.0% which tends to believe the cornerstone of diabetes care [4,5].
Regarding diabetes and hypoglycemia, the current kinds of literature evidence revealed that worldwide, more than 284 million people have diabetes, and this number is expected to reach 439 million by 2030 approximately 90% of these people have type 2 diabetes as a result the number of hypoglycemic cases expected to be increased as well [6].
Hypoglycemia is also a common adversative event in people with type 1 diabetes and type 2 diabetes mellitus (T2DM) treated with insulin and/or oral hypoglycemic agents [7]. It is a rate-limiting complication in the achievement of strict glycemic control in diabetes management and significant episodes of hypoglycemia and its attendant counter-regulatory hormonal response lead to poor glycemic control diabetes mellitus [8].
Hypoglycemia symptoms were confirmed to be a predictor of fatigue, consequently, it is essential to consider age and disease duration, and regarding the magnitude about, up to 60% of patients with diabetes experience fatigue symptoms [9-12]. Poor glycemic control leads to kidney damage, and measures of cognitive and functional impairments were strongly associated with an increased risk of severe hypoglycemia [12].
Therefore to prevent the effects of hypoglycemia attention to diagnose diabetes mellitus early and prevent associated complications, ultimately improving knowledge improving lifestyles, and removing bad habits among diabetes mellitus patients.
Hypoglycemia has been considered a major barrier to achieving the proper glycemic objective in diabetes mellitus patients. In precise, severe hypoglycemia (SH), which is well-defined as a hypoglycemic occurrence requiring the assistance of another person to raise the patient’s glucose level, is a grave problem of diabetes because of its possible serious consequences [9,13].
Severe hypoglycemia is one of the strongest predictors of adverse clinical outcomes in patients with diabetes and recent research findings indicated that glycemic control does not reduce cardiovascular disease mortality among diabetic patients but poor glycemic control leads to starvation of vital organs as a result predisposes to early and preventable death [14,15]. Hypoglycemia causes a devastating form of organ failure leading to severe morbidity and mortality and the mortality rate due to severe hypoglycemia was 10.1% [16].
Even though the magnitude of previously undiagnosed diabetes mellitus was 88.5%, the magnitude of diabetes was found to be 15.9% which in turn leads to the acute complication of DM [17].
Studies in East African countries showed that the magnitude of poor glycemic control(hypoglycemia) tends to increase from 30% to 70.5% [18]. Internationally as well as national efforts have been made to minimize and reduce the effects of diabetes mellitus and its complication hypoglycemia through education of DM patients regarding knowledge on symptoms of hypoglycemia, precipitating factors, remedial measures during sign symptoms of low blood glucose or hypoglycemic state, and since there is a knowledge gap on important aspects of hypoglycemia among diabetic patients [8,19].
It is well known that Effective blood glucose control is the foundation of diabetes management aimed at minimizing microvascular and macrovascular complications but the risk of hypoglycemia increases when glucose control is intensified and this can act as a barrier to achieving blood glucose targets [6]. However, the clear mechanism of insulin as well as oral hypoglycemic agents to reduce significantly blood glucose levels with standard dose and the mechanism of dementia due to hypoglycemia and the process of hypoglycemia without any common disorders are unclear and should be studied further [20-22].
Influences like poor glycemic control, glycemic variability as captured by 1,5-anhydroglucitol, kidney damage, and measures of cognitive and functional impairments were issues that destructively affect an increased hazard of severe hypoglycemia [23]. Hypoglycemic control is also positively affected by death, poor glycemic control increases death risk by 266%, and mortality in non-intensive care unit diabetes mellitus patients with contagions is also another factor vice versa to causes death [16].
There is strong evidence that diabetes mellitus increases the risk of cognitive impairment and dementia. Insulin signaling dysregulation and small vessel disease in the base of diabetes may be important contributing factors in Alzheimer’s disease and vascular dementia pathogenesis, respectively [9].
Notwithstanding numerous efforts made to reduce the effects of diabetes and hypoglycemia, problems concerning the knowledge and practice of patients as well as healthy individuals regarding hypoglycemia are not satisfactory and the effects of hypoglycemia are not diminished well. Therefore further study should be suggested to recognize the root cause of the problems related to hypoglycemia.
The research conducted on the assessment of hypoglycemia is very rare even the research conducted on this issue does not reveal the whole assessment of hypoglycemia. But the current study tries to assess the prevalence of hypoglycemia and its associated factors plus knowledge, attitude, and practice of type 1 DM patients, and this finding will give the overall assessment of hypoglycemia other than other studies
Since hypoglycemia is a major health problem and is sustained to death it should be properly managed but researchers do not properly recommend it for health institutions this research will fill this gap by appropriate recommendation of findings with possible solutions.
Therefore the study will provide relevant information, for health care administrators communities, and authorized bodies to create awareness for the early identification of problems related to hypoglycemia through health education and health promotion.
The research findings will also be an important alarm to the community for early recognition of the problem and to prevent the problem as to increase health-seeking behavior other than complaining and being worried.
For researchers -the study is also used as supplementation and reference who want to conduct similar research which it deserves finally, the research paper will be sent to different journals for publication.
Study area and period
The study was carried out at Debre-Tabor Comprehensive Specialized Hospital from October 1/2020 - March 30/2021. Debre-Tabor is located northwest of the Amhara Region of Ethiopia, 103km from Bahir Dar (Regional Capital), and 666 km from Addis Ababa (Capital city of Ethiopia). It is one of the oldest hospitals in the Amhara region, which provides services for about five million populations. The hospital is currently used as a referral center for district hospitals in the zone and a teaching hospital for medical and health science students of Debre-Tabor University.
Study design
The institution-based cross-sectional quantitative study was employed.
Sources population
All diabetes mellitus patients were attending the outpatient clinic atDTCSH.
Study population
All type I DM patients who have a list of registration with each follow-up date and found at DTCSH, OPD clinic at the time of data collection and who fulfill the inclusion criteria were the study populations.
Sampling unit
Several diabetic clinic OPDs selected from other OPDs were the sampling units.
Eligibility criteria
Inclusion criteria: Underwent Type I DM for at least 3 months before the study and had regular DM follow-up, with or without comorbidities and Age of the patient≥ 18 years
Exclusion criteria: Documented mental disabilities having any speech impairment and Incomplete charts and patient files
Sample size determination
To calculate the sample size for the current study prevalence of hypoglycemia from a similar study in Ethiopia will be taken and the related article was considered. In this study, the sample size was determined by using a single population proportion formula as follows.
n0 = 185
n0 = 185
By adding a 10% none response rate the total sample size is
nf = 185+18.5
nf = 203.5
The total sample size = 204
Where:
n0 = i nitial sample size
nf = the desired sample size(final sample size)
P = prevalence of hypoglycemia in Hawassa University Comprehensive Specialized Hospital, Ethiopia (14%) [24].
Zα/2 = standard normal variation value at a confidence interval of 95% (1.96)
d = the margin error between the sample and the population
Sampling technique and sampling procedure
A systematic random sampling technique was utilized to select type 1DM patients that have a chronic follow-up at DTCSH, The sampling interval “K” value was calculated as K = N/n, by considering 2 months data and Kth value =N/n=~2, therefore, the data will be collected every 2 intervals from the queue of patients from follow up registration. Thus using patients’ record order which was listed in the follow-up appointment as the sampling frame, participants were selected in every 2 number intervals until reaching the total sample size, and the first participant was selected by the lottery method.
Data collection tools and procedures
Data was collected using validated interview-based and checklist-related questionnaires. The questionnaire contains socio-demographic characteristics, knowledge, attitude, and practice of hypoglycemia among T1DM. The questionnaires also contain prevalence, monitoring, and assessment of hypoglycemia. Data was also collected by using both open-ended and closed-ended questionnaires among type 1 DM who had a regular follow-up in DT comprehensive specialized hospital. The questionnaires were prepared by adopting validated articles before starting the interview the questionnaires primarily being prepared in English and then translated into the local language (Amharic) for its consistency and understandability to the patients in whom this research was conducted. During translation, all the concerns and the local linguistics were put into consideration and the local language (Amharic) will be translated back to English for the appropriateness and conformability of analysis of the findings of the research. A pretest was conducted among 5% of the participants from Dessie Comprehensive Specialized Referral Hospital and modification was considered according to its findings. After modification and amendment, the data was collected by face-to-face interviews with two trained nurses after they obtained a one-day training on the tools and necessary care needed. The parents were interviewed at the DM clinic in Debre-Tabor Comprehensive Specialized Hospital.
Variables of the study
Dependent variables: Prevalence of hypoglycemia
Independent variables
Sociodemographic related factors: Age, Sex, Religion, Occupation, education, Residence, Income, Marital status, Duration of Diabetes mellitus, KAP towards hypoglycemia BGL
Operational definitions and terms
Hypoglycemia: When blood sugar levels are <75 milligrams per deciliter (39)
Good knowledge: A score of knowledge > 60% on the knowledge assessment questions [25]
Poor knowledge: A score of < 60% on the knowledge assessment questions [25]
Good practice: A score of > 60% on the practice assessment questions [25].
Poor practice: A score of < 60% on the practice assessment questions [25].
Favorable attitude: a mean and above score of participants from the attitude questions towards diabetes mellitus [26].
Unfavorable attitude: less than the mean score of participants from the attitude questions towards diabetes mellitus [26].
Data quality control
Data collection was supervised for the correct implementation of procedures by supervisors and the investigator. The completeness and consistency of the questionnaire were also checked at the end of data collection.
Data analysis and processing
After the data collection, the response was coded and entered into a computer by using EPI-info data version 7 statistical packages, and 10% of the responses were randomly selected and checked for the consistency of the data entry. SPSS version 20 was also used for data analysis. Frequency and Percentage were calculated for all variables that are related to the objective of the study, and Bivariate and multivariable logistic regression was employed to identify factors associated with dependent variables. Odds ratio (OR), with 95% CI and p value < 0.05 were computed to determine the level of significance.
Data dissemination plan
A copy of the report will be given to Debre-Tabor Comprehensive Referral Hospital and other concerned bodies. It is also expected that the result of this study will be disseminated to the public through the media. Additionally, the result may be presented at scientific conferences and published in scientific journals.
Ethical consideration
Ethical clearance was obtained from the institutional review board (IRB) of Debre-Tabor University. A written letter of permission from the research coordination committee was submitted to the Debre-Tabor comprehensive referral Hospital administration to grant permission to conduct the study. The study participants were provided with clear information about the purpose of the study and asked if they were willing to participate in the study. Data was collected after receiving verbal consent from those who were willing to participate in the study. The anonymity of the respondents was preserved and their information was kept secret and was not disclosed to anyone except for the study.
Socio-demographic characteristics of the respondents
A total of 204 participants were approached and 204 of them agreed to participate giving a response rate of 100%. Of the participants, more than half of them 104 (51.0%) were females. The majority of the study participants, 25% (51) were found in the age group of 18-25 years whereas the mean age and monthly income of the respondents were 39.451 ± 15.4 and 3057.57 ± 2503.36 respectively. Regarding their occupational status, about one-third, 31.9% (65) were farmers whereas more than half, 52.9% (108) had no formal education.
Out of the study participants, about 58.8% (120) of the respondents are urban dwellers and of them 64.2% (131) are married by their marital status Regarding income status 44.6% (91) of the study participants earn 500-1500 ETB monthly income.
Regarding the duration of diabetes mellitus 56.9% (116) of the respondents live with DM 1-3 years whereas a few of them, 5.4% (11) of the study participants live with DM >10 years (Table 1).
| Table 1: Socio-demographic characteristic of type1 diabetes mellitus patients attending the outpatient clinic of DTCSH Northwest Ethiopia, 2021 (N = 204). | |||
| Variable | Category | Frequency(N) | Percentage (%) |
| Age(Years) | 18-25 | 51 | 25 |
| 26-35 | 47 | 23 | |
| 36-45 | 39 | 19.1 | |
| 46-55 | 31 | 15.2 | |
| >56 | 36 | 17.6 | |
| Sex | Male | 100 | 49 |
| female | 104 | 51 | |
| Religion | Orthodox Christian | 180 | 88.2 |
| Protestant | 14 | 6.9 | |
| Muslim | 8 | 3.9 | |
| Catholic | 1 | 0.5 | |
| Adventist | 1 | 0.5 | |
| Occupational status | House wife | 54 | 26.5 |
| Farmer | 65 | 31.9 | |
| Government inquiry | 30 | 14.7 | |
| NGO employ | 12 | 5.9 | |
| Private business | 43 | 21.1 | |
| Educational level | No formal education | 108 | 52.9 |
| Can read and write | 15 | 7.4 | |
| Primary level | 12 | 5.9 | |
| Secondary level | 29 | 14.2 | |
| Higher education | 40 | 19.6 | |
| Residence | Urban | 120 | 58.8 |
| Rural | 84 | 41.2 | |
| Marital status | Never married | 51 | 25 |
| Married | 131 | 64.2 | |
| Widowed | 18 | 8.8 | |
| Divorced | 4 | 2 | |
| Monthly income | < 500 | 18 | 8.8 |
| 500-1000 | 91 | 44.6 | |
| 1001-1500 | 66 | 32.4 | |
| 1501-2000 | 17 | 8.3 | |
| > 2000 | 12 | 5.9 | |
| Duration of type 1 Diabetes mellitus | < 1 years | 30 | 14.7 |
| 1-3 Years | 116 | 56.9 | |
| 3-5 Years | 35 | 17.2 | |
| 5-10 years | 12 | 5.9 | |
| > 10 years | 11 | 5.4 | |
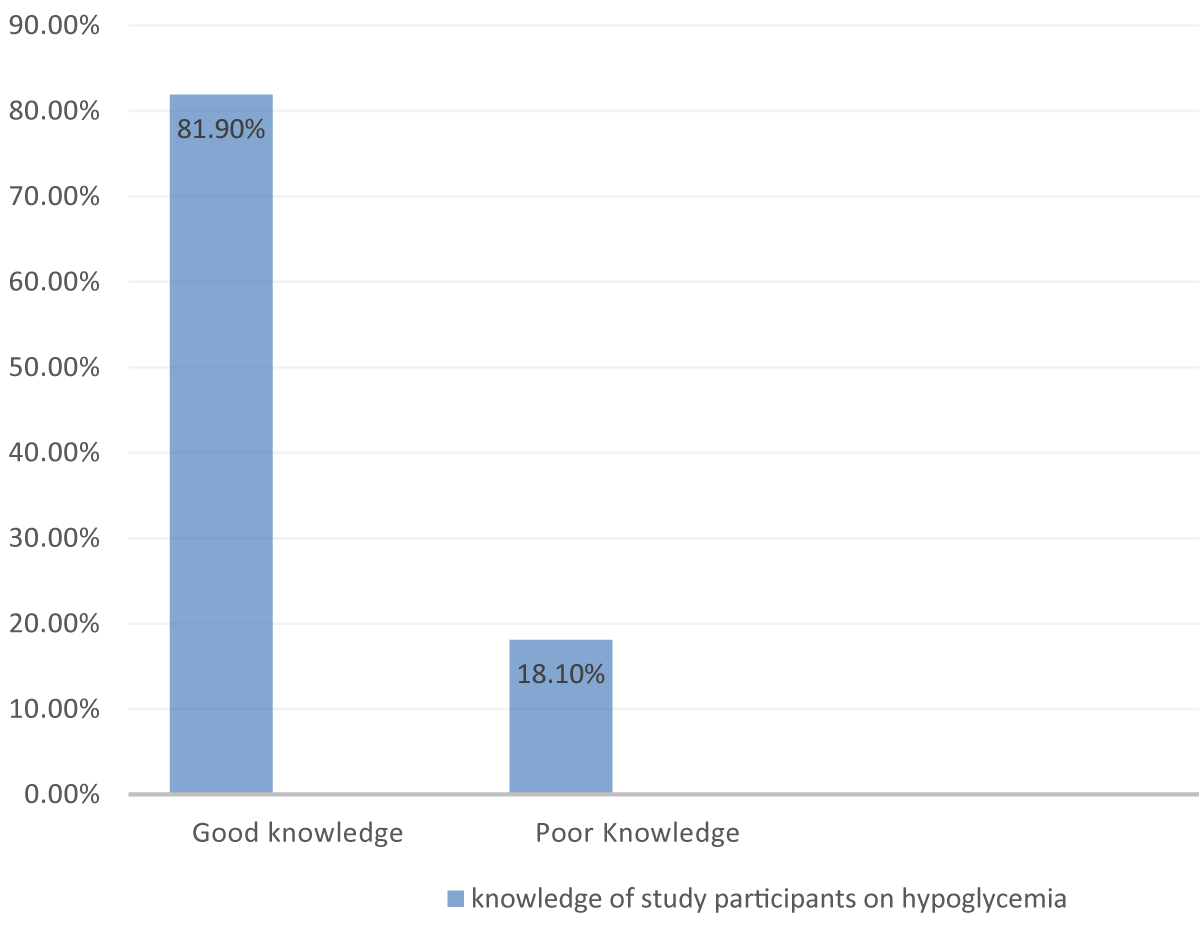
Knowledge of type DM patients about hypoglycemia
The overall knowledge of the respondents was found to be 81.9% (95%, CI, 76%-86.8%), and more than half, 51.5% (105) responded positively as diabetes mellitus means high blood sugar how ever higher respondents, 96.1% (196) knew about insulin whereas 93.6% (191) of the respondents prevail that Insulin vial should store in the refrigerator or cold place.
Regarding how to take insulin injections, 94.1% (192) responded that insulin injections should be taken soon after or just before taking food. Similarly, about 96.6% (197) of the study participants knew that the proper site for injection is the abdomen and in the same way, 57.4% (117) respondents responded that the angle to administer insulin is 45 degrees.
Of the respondents, 58.8% (120) distinguish the distance to rotate on the same site as one thumb whereas 87.3% (178) also see the complication of insulin therapy. About 87.7% (178) of respondents know the use of rotation of the injection site to reduce pain and prevent wasting of subcutaneous tissue (Table 2).
| Table 2: knowledge of type1 diabetes mellitus patients attending the outpatient clinic of DTCSH, Northwest Ethiopia, 2021 (N = 204). | |||
| Knowledge of type1 diabetes mellitus patients domain | Category | Frequency (N) | Percentage (%) |
| Diabetes mellitus means high blood sugar | Yes | 105 | 51.5 |
| No | 99 | 48.5 | |
| Know about insulin | Yes | 196 | 96.1 |
| No | 8 | 3.9 | |
| Insulin vial is stored in the refrigerator or cold place | Yes | 191 | 93.6 |
| No | 13 | 6.4 | |
| Insulin injection is taken soon after or just before taking food | Yes | 192 | 94.1 |
| No | 12 | 5.9 | |
| The sites for insulin injection are abdomen, thigh, glutei and deltoid | Yes | 197 | 96.6 |
| No | 7 | 3.4 | |
| The angle to administer insulin is 45 degree | Yes | 117 | 57.4 |
| No | 87 | 42.6 | |
| The distance to rotate on the same site is one thumb | Yes | 120 | 58.8 |
| No | 84 | 41.2 | |
| Ways to reduce pain during insulin injection are inters the skin, do not manipulate the needle once inserted, avoiding re using of the same site | Yes | 173 | 84.8 |
| No | 31 | 15.2 | |
| The complications of insulin therapy are low blood sugar, insulin resistance and wasting of subcutaneous tissue | Yes | 178 | 87.3 |
| No | 26 | 12.7 | |
| The use of rotation of the injection site is to reduce pain, prevent wasting of subcutaneous tissues | Yes | 179 | 87.7 |
| No | 25 | 12.3 | |
| Massage after injection is used to enhances the rapid absorption of insulin | Yes | 158 | 77.5 |
| No | 46 | 22.5 | |
| The benefit of insulin self-administration are, time saving, inexpensive and easy to take on self while traveling | Yes | 182 | 89.2 |
| No | 22 | 10.8 | |
About 77.5% (158) of respondents respond that massaging after injection is used to enhance the rapid absorption of insulin whereas 89.2% (182) recognize the benefits of insulin self-administration (Figure 1).
Figure 1: Knowledge of study participants of hypoglycem at DTCSH, 2021.
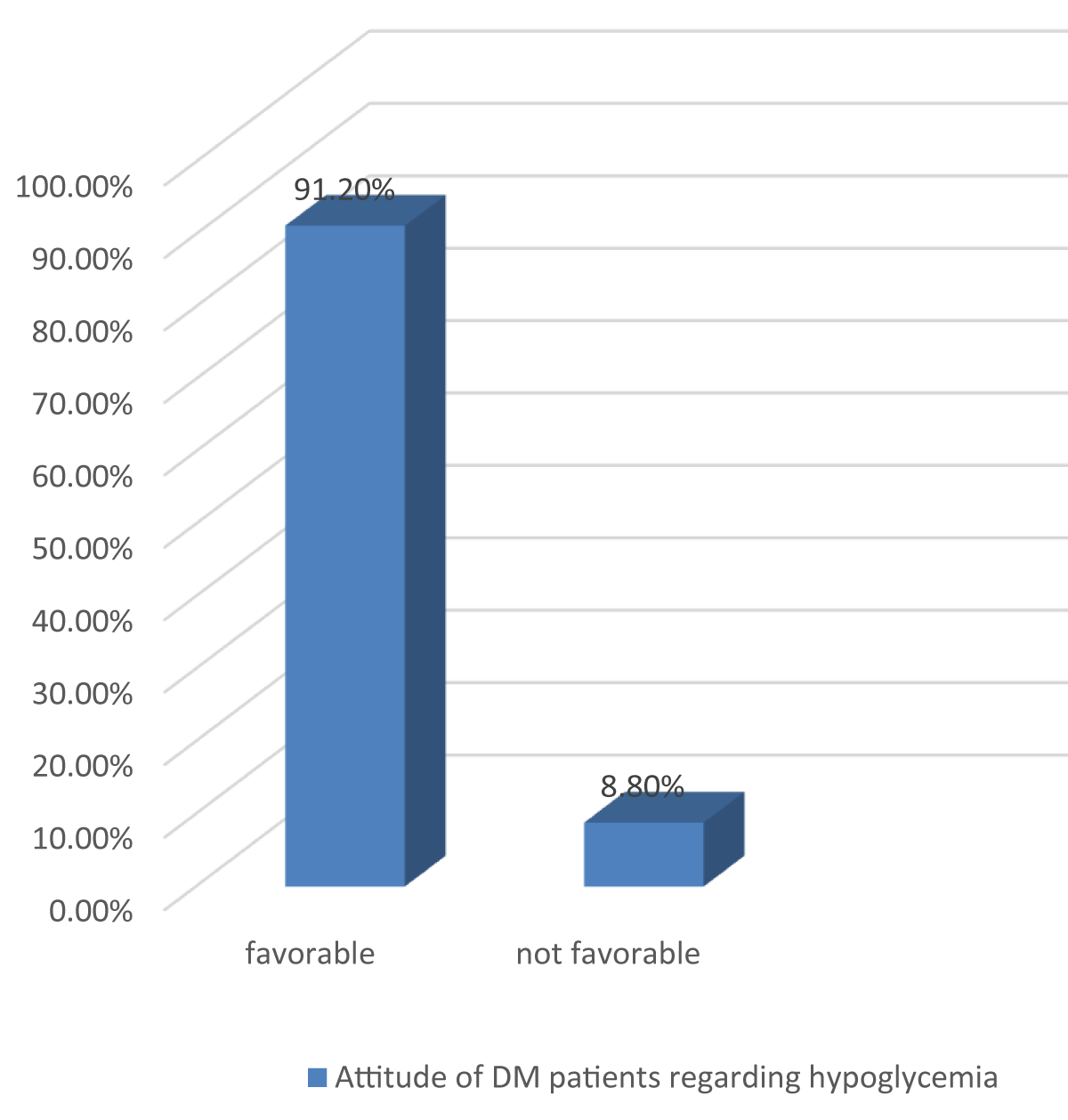
The attitude of DM patients regarding hypoglycemia
The attitude of the respondents is favorable with the total attitude score 91.2% (95% CI, 86.8-94.6) (Figure 2). Of the overall respondents 89.7% (183) agree with the assumption insulin causes other health problems whereas a similar amount of study participants agree that the averseness of insulin self-administration decreases blood glucose levels and 89.2% (182) respondents also agree that insulin self-administration does not bring stigma whereas 98.2% (201) also agree that self-administering of insulin helps to reduce cost and time (Table 3).
Figure 2: Attitude of DM patients regarding hypoglycemia at DTCSH, 2021.
| Table 3:Attitude of type1 diabetes mellitus patients attending the outpatient clinic of DTCSH, Northwest Ethiopia, 2021 (N = 204). | |||
| Attitude of type1 diabetes mellitus patients domain | Category | Frequency (N) | Percentage (%) |
| Insulin causes other health problems |
Agree | 183 | 89.7 |
| Disagree | 19 | 9.3 | |
| Neutral | 2 | 1.0 | |
| Insulin self-administration decreases blood glucose | Agree | 183 | 89.7 |
| Disagree | 21 | 10.3 | |
| Insulin self-administration is not tiresome | Agree | 183 | 89.7 |
| Disagree | 21 | 10.3 | |
| Insulin self-administration does not brings stigma | Agree | 182 | 89.2 |
| Disagree | 20 | 9.8 | |
| neutral | 2 | 1.0 | |
| Insulin self-administration is beneficiary regarding cost and time | Agree | 201 | 98.5 |
| Disagree | 3 | 1.5 | |
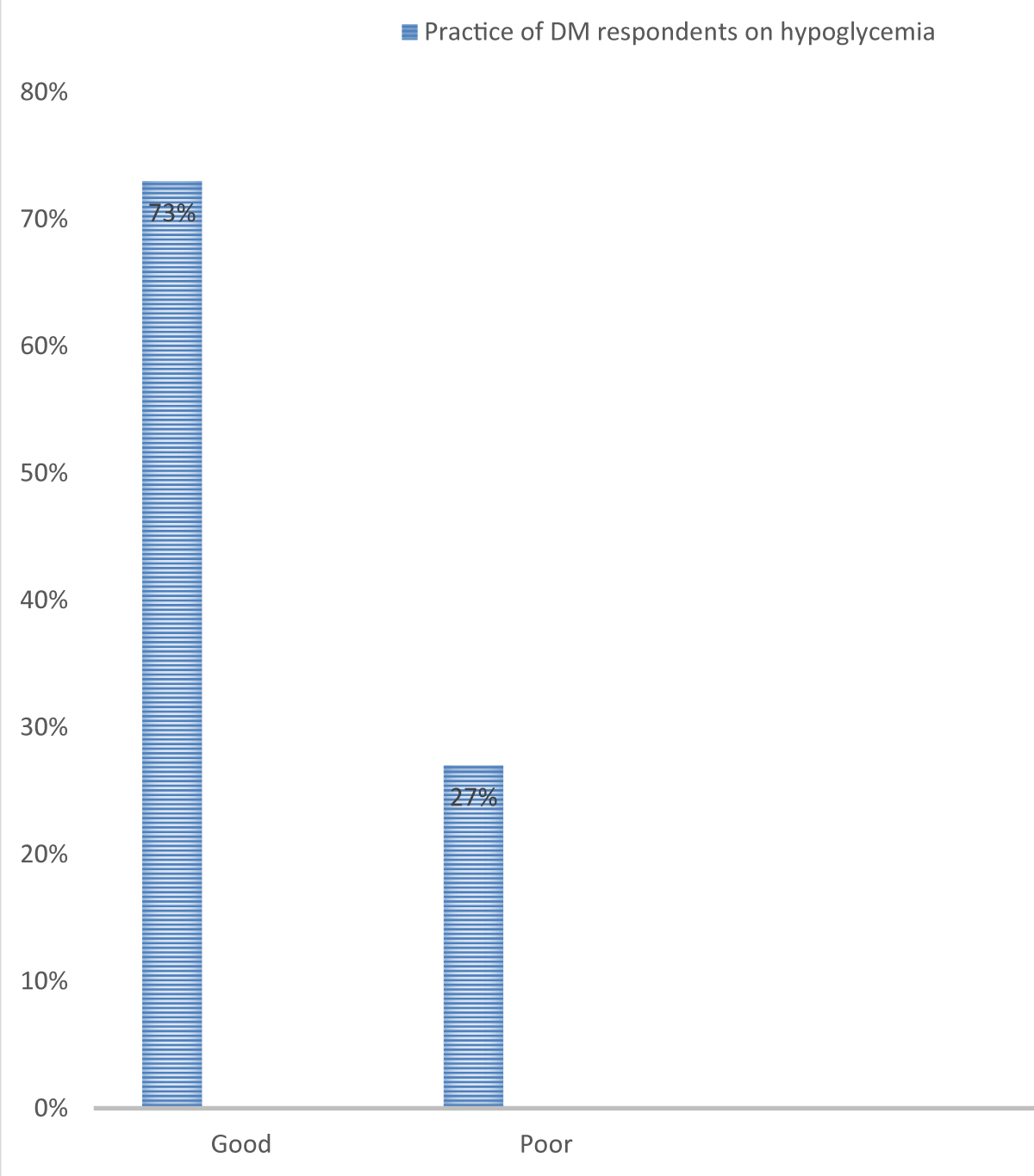
The practice of DM respondents on hypoglycemia
The practice of the respondents is poor with a total poor practice score of 73% (95% CI, 66.7-78.9) (Figure 3). Of the total respondents, 35.8% (73) can inject insulin by themselves but only 25.5% (52) study participants inject insulin at 45°. From total insulin users 29.4% (60) store insulin vials in a refrigerator or cold place.
Figure 3: Practice of DM respondents on hypoglycemia at DTCSH, 2021.
Similarly from insulin injection users, 24.3% (50) did not frequently repeat injection sites but 11.3% (23) frequently repeat the injection sites. Regarding insulin administration, 24.5% (50) did not inject insulin before or immediately after food intake whereas 22.1% (45) injected insulin into their abdomen, thigh, gluteus, or deltoid areas (Table 4).
| Table 4: Practice of type1 diabetes mellitus patients attending the outpatient clinic of DTCSH,Northwest Ethiopia, 2021 (N = 204). | |||
| Practice of type1 diabetes mellitus patients domain | Category | Frequency (N) | Percentage (%) |
| Can you inject yourself in correct position? | Yes | 73 | 35.8 |
| No | 131 | 64.2 | |
| Do you inject yourself with needle at 45° | Yes | 52 | 25.5 |
| No | 21 | 10.3 | |
| Do you store insulin vials in refrigerator or cold place? | Yes | 60 | 29.4 |
| No | 13 | 6.4 | |
| Do you frequently repeat injection sites? | Yes | 23 | 11.3 |
| No | 50 | 24.5 | |
| Do you inject insulin before or immediately after food Intake? | Yes | 23 | 11.3 |
| No | 50 | 24.5 | |
| Do you inject insulin into abdomen, thigh, gluteus or deltoid? |
Yes | 45 | 22.1 |
| No | 28 | 13.7 | |
Assessment of the prevalence of hypoglycemia
The prevalence of hypoglycemia is high with a total score of 88.7% (95%, CI 83.8-92.6). (Figure 4). Of the overall study participants, 93.1% (190) were aware of hypoglycemia by self as well as by relatives regarding its treatment. Diabetic patients who faced hypoglycemia in the three months was 25.4% (46) followed by 34.3% (70) finding different solutions with no treatment assistance. However, 86.8% (177) of the respondents came to the diabetic clinic for the reason of follow-up.
Figure 4: Prevalence of hypoglycemia at DTCSH, 2021.
Of the total diabetic patients, 89.5% (201) took the prescribed medications insulin as well as oral hypoglycemic agents, however, the majority of the DM patients, 64.2% (131) took oral hypoglycemic agents. The majority of the respondents, 95% (194) administer DM medications like insulin and oral hypoglycemic agents by themselves whereas 9.8% (20) do not take insulin at regular times. Among insulin users, 7.4% (15) took a higher dose whereas 28.4 (54) of the respondents took the normal dose.
Regarding food consumption, missed /hungry 49% (100), with medication 25%(51), physical activity with food 48% (98),physical activity without food 14.7% (30), alcohol consumption with food 11.3%(23) and alcohol consumption without food 7.8% (16) .
Concerning comorbidity 12.3% (25) had the disease in addition to DM whereas 6.5% (13) of the study participants are members of the DM association (Table 5).
| Table 5: Assessment on the prevalence of hypoglycemia among type1 diabetes mellitus patients attending the outpatient clinic of DTCSH,2021, Northwest Ethiopia, 2021 (N = 204) | ||||
| Assessment on the prevalence of hypoglycemia of type1 diabetes mellitus patients domain | Category | Frequency (N) | Percentage (%) | |
| Awareness of low blood glucose levels by the respondents and relatives. | Yes | 181 | 88.7 | |
| No | 23 | 11.3 | ||
| Awareness of hypoglycemia by the Pt and relatives and its treatment | Yes | 190 | 93.1 | |
| No | 14 | 6.9 | ||
| Frequency of hypoglycemia in the three months |
Once | 37 | 18.1 | |
| Twice | 37 | 18.1 | ||
| Three times | 46 | 25.4 | ||
| Four times | 54 | 26 | ||
| Five and above times Never happened |
16 |
7.8 | ||
| Solutions the events of hypoglycemia in the last three months | No treatment assistance needed | 70 | 34.3 | |
| Taking rest but no assistance needed | 65 | 31.9 | ||
| Treatment with the assistance of a third party needed | 55 | 27 | ||
| Reasons coming to the diabetic clinic | Follow up-to diabetes mellitus Another personal issue |
177 87 |
86.8 13.2 |
|
| Taking the prescribed medication since you were | Yes | 201 | 98.5 | |
| diagnosed with DM | No | 3 | 1.5 | |
| Types of medication taken by the patients /relatives | Regular insulin (the clear one in color) | 15 | 7.4 | |
| NPH insulin (the cloudy one in color) | 20 | 9.8 | ||
| Both | 35 | 17.2 | ||
| Oral hypoglycemic agent | 131 | 64.2 | ||
| Responsible body to administer medication | My self | 194 | 95 | |
| Family | 7 | 5 | ||
| Insulin Administration | Not taking in regular time |
Yes | 20 | 9.8 |
| No | 53 | 26 | ||
| Taking Higher dose | Yes | 15 | 7.4 | |
| No | 58 | 28.4 | ||
| Food consumption | Missed/hungry | Yes | 100 | 49 |
| No | 81 | 39.7 | ||
| With medication | Yes | 51 | 25 | |
| No | 130 | 63.7 | ||
| Physical activity with food | Yes | 98 | 48 | |
| No | 83 | 40.7 | ||
| Physical activity out of food | Yes | 30 | 14.7 | |
| No | 151 | 74 | ||
| Alcohol consumption with food | Yes | 23 | 11.3 | |
| No | 158 | 77.5 | ||
| Alcohol consumption without food | Yes | 16 | 7.8 | |
| No | 165 | 80.9 | ||
| When you feel ill with another disease in addition to DM |
Yes | 25 | 12.3 | |
| No | 179 | 87.7 | ||
| Members sheep of Ethiopian DM association | Yes | 13 | 6.4 | |
| No | 191 | 93.6 | ||
Assessment on Self-monitoring of blood glucose (SMBG) and management of hypoglycemia
Regarding self-monitoring of blood glucose (SMBG) 25.5% (52) of the respondents revealed that they can monitoring of blood glucose levels at home. Of the 17.2% (35) of the study participants have blood glucose monitoring during follow-up from the DM clinic. From DM patients who have a glucometer, having ≥ 3 times/week BGL monitoring was 2% (4).
Regarding ways of preventing hypoglycemia about 25.5% (52) of respondents checked their blood glucose level and 29.4% (60) of DM patients taking/giving sweet candies to manage hypoglycemia (Table 6).
| Table 6: Assessment on Self-monitoring of blood glucose (SMBG) and management of hypoglycemia among type1 diabetes mellitus patients attending the outpatient clinic of Debre -Tabor Compressive and Specialized Hospital, Northwest Ethiopia, 2021 (N = 204). | |||
| Assessment on Self-monitoring of blood glucose (SMBG) and management of hypoglycemia of type1 diabetes mellitus patients domain | Category | Frequency(N) | Percentage(%) |
| Monitoring of blood glucose level at home |
Yes | 52 | 25.5 |
| No | 152 | 74.5 | |
| Mechanism of monitoring blood glucose level | Using my glucometer | 10 | 4.9 |
| Follow up to my clinic | 35 | 17.2 | |
| Home care doctor/ nurse | 7 | 3.4 | |
| Frequency of blood glucose level by glucometer/week | 1 | 2 | 1 |
| 2 | 4 | 2 | |
| ≥ 3 | 4 | 2 | |
| Way of preventing hypoglycemia |
Checking my/his/her blood glucose | 52 | 25.5 |
| Maintain my/his/her physical activity | 21 | 10.3 | |
| Adjusting my/his/her regular meal/snack | 51 | 25 | |
| Maintain my/his/her physical activity | 10 | 4.9 | |
| Seeking medical advice from a health professional | 47 | 23 | |
| Possibilities used as immediate management of hypoglycemia by the Pt/ partner |
Taking/giving fruit juice | 13 | 6.4 |
| Taking/giving soft drinks | 55 | 27 | |
| Taking/giving sweet candies | 60 | 29.4 | |
| Taking/giving table sugar | 30 | 14.7 | |
| Taking/giving honey | 8 | 3.9 | |
| Call to ambulance/go to a nearby clinic | 15 | 7.4 | |
Findings from chart review
From the chart review, the mean fasting blood sugar in recent times was 72.42 ± 83.26 followed by fasting blood sugar on the immediate previous appointment 154 ± 92.35, and on the second previous appointment (immediately before the previous appointment) 177 ± 360 (Table 7).
| Table 7: Findings from chart review. | ||
| Variables | Mean | Standard deviation |
| Fasting blood glucose value | ||
| Recent | 72.42 | 83.26 |
| On immediate previous appointment | 154 | 92.35 |
| On second previous appointment (immediately before the previous appointment) | 177 | 360 |
| Anthropometric data | ||
| weight (Kg) | 59.42 | 8 |
| height (cm) | 120 | 104 |
| BMI | 22.42 | 11.57 |
Factors associated with the prevalence of hypoglycemia among DM patients
The factorial analysis was conducted by using Spss version 20 and the binary logistic regression model was used for the analysis of COR and AOR. A logistic regression model was used to test the presence or absence of association between dependent and independent variables.
Factors associated with the prevalence of hypoglycemia among DM patients were identified and the variables with a p - value of 0.20 and less would fit the logistic model for multivariable analysis to determine the relative prediction level of independent variables to the outcome variable. p – value less than or equal to 0.05 with 95% CI had been considered statistically significant.
Model goodness-of-fit would be checked by the Hosmer Lemeshow test, which shows the model fitness was 90.8% at multivariable analysis, which indicates the model fitness was good. Model fitness was also checked by the chi-square test at the Pearson chi-square test, which also revealed the significance level of the variable, which shows a significant association between dependent and independent variables, and the significance level was 0.003.
Variables that had a p - value less than 0.2 and variables were respondents with the occupation of housewife [COR: 4.37 (95% CI:1.24-9.53], educational level of no formal education [COR: 2.3 (95% CI:1.8-8.4] and marital status of never-married [COR: 3.0 (95% CI:2.6-13.3] had positively associated with the outcome variable at Bivariable analysis whereas variables such as residence of respondents urban [COR: 0.83 (95% CI:2.2-10.22], duration of diabetes mellitus < 1 year[COR: 0.89 (95% CI:1.8-12.00], good knowledge of parents [COR: 0.67 (95% CI:1.7-15.0], good practice [COR: 0.9 (95% CI:2.9-18.0], favorable attitude [COR: 0.65 (95% CI:3.6-18.0] and monitor BGL [COR: 0.44 (95% CI:1.6-20.0] were negatively associated with the outcome variable from the Bivariable analysis and that variable were exported to multi-variable analysis. Among the candidate variables for multi-variable analysis residence, marital status, the practice of the respondents, and monitoring of blood glucose levels were eliminated by the final stage of multi-variable analysis but the occupation of housewives [AOR:4.0 (95% CI:1.86-9.35)], and educational level of no formal education [AOR: 2.1 (95% CI:1.9-13.1)] were statistically significantly associated with the outcome variable at multivariable analysis whereas variables such as duration of diabetes mellitus < 1 year [AOR: 0.8 (1.3-9.28)], good knowledge of parents [AOR: 0.9 (1.09-11.0)] and favorable attitude [AOR: 0.86 (1.1-6.0)] were negatively associated with the outcome variables. The prevalence of hypoglycemia was affected 4 times by the occupation of the housewife than in private business [AOR: 4.0 (1.86-9.35)] whereas study participants who have no formal education increased the risk factors of hypoglycemia by 2.1 times than respondents who have higher educational status [AOR: 2.1 (1.9-13.1)].
However, study participants who had diabetic duration < 1 year reduced the risk of hypoglycemia by 20% when compared with the duration of diabetes>10 years [AOR: 0.8 (1.3-9.28)]. Similarly, participants who have good knowledge and favorable attitude also reduce the prevalence of hypoglycemia by 10%, [AOR: 0.9 (95% CI:1.09-11.0)] and 14%, [AOR: 0.86 (1.1-6.0)] respectively when compared with poor knowledge and unfavorable attitude (Table 8).
| Table 8:Factors associated with the prevalence of the hypoglycemia among type1 diabetes mellitus patients attending the outpatient clinic of DTCSH, Northwest Ethiopia, 2021 (N = 204). | ||||
| Variables | Prevalence of hypoglycemia | COR | AOR | |
| Yes | No | |||
| Occupation | ||||
| Housewife | 35(2.5%) | 19(9.3%) | [COR: 4.37(1.24-9.53] | [AOR:4.0(1.86-9.35)] |
| Farmer | 40(19.6%) | 20(9.8%) | [COR:1.53(1.52-18.63] | [AOR:1.3(1.7-.3.7)] |
| Government inquiry | 22(10.8%) | 8(3.9%) | [COR:0.5.(0.2-11.3] | AOR:0.33(0.7-.3.53)] |
| NGO employ | 10(4.9%) | 2(1%) | [COR:0.8.(0.82-11.0] | AOR:1.00(0.9-.7.2)] |
| Private business | 30(14.7 %) | 13(6.4%) | 1 | 1 |
| Educational level | ||||
| No formal education | 69(33.8%) | 39(19.1%) | [COR: 2.3(1.8-8.4] | [AOR:2.1(1.9-13.1)] |
| Can read and write | 10(4.9%) | 5(2.5%) | [COR: 1.81.(22-10.3] | [AOR:2.0(0.6-.9.2)] |
| Primary level | 10(4.9%) | 2(1%) | [COR: 0.26(0.73-6.23] | [AOR:0.32(0.7-5.66)] |
| Secondary level | 19(9.3%) | 10(4.9%) | [COR: 0.27(0.5-7.35] | [AOR:0.2(0.3-.4.22)] |
| Higher education | 30(14.7%) | 10(4.9%) | [COR: 1.56(0.66-7.12] [COR: 0.6(0.43-6.2] 1 |
[AOR:2.11(1.7611.35)] [AOR:0.54(0.53-7.2)] 1 |
| Residence | ||||
| Urban | 90(44.1%) | 30(16.7%) | [COR: 0.83(2.2-10.22] | [AOR: 0.7(0.93-12.0)] |
| Rural | 64(31.4%) | 20(4%) | 1 | 1 |
| Marital status | ||||
| Never married | 31(1.5%) | 20(9.8%) | [COR: 3.0(2.6-13.3] | [AOR: 2.5(0.67-8.3)] |
| Married | 101(49.5%) | 30(14.7%) | [COR: 0.72(0.77-14.0] | [AOR: 0.8(0.75-12.0)] |
| Widowed | 13(6.4%) | 5(2.5%) | [COR: 0.4(0.5-8.65] | [AOR:0.0(0.7-10.55)] |
| Divorced | 3(1.5%) | 1(0.5%) | [COR: 0.77(0.67-5.65] 1 |
[AOR:0.5(0.65-7.44)] 1 |
| Duration of Diabetes mellitus | ||||
| <1 year | 23(11.3%) | 7(3.4%) | [COR: 0.89(1.8-12.00] | [AOR: 0.8(1.3-9.28)] |
| 1-3 Years | 106(52%) | 10(4.9%) | [COR: 1.5(0.46-8.75] | [AOR:2.0(0.67-10.0)] |
| 3-5 Years | 30(14.7%) | 5(2.5%) | [COR: 2.4(0.6-9.77] | [AOR:2.6(0.92-13.0)] |
| 5-10 years | 9(4.4%) | 3(1.5%) | [COR: 6.2(0.87-14.87] | [AOR:6.1(0.87-17.00)] |
| >10 years | 8(3.9%) | 2(1%) | 1 | 1 |
| Knowledge | ||||
| Good | 140(68.6%) | 27(13.2%) | [COR: 0.67(1.7-15.0] | [AOR: 0.9(1.09-11.0)] |
| Poor | 30(14.7%) | 7(3.4%) | 1 | 1 |
| Practice | ||||
| Good | 44(21.6%) | 11(5.4%) | [COR: 0.9(2.9-18.0] | [AOR: 0.87(0.67-8.0)] |
| Poor | 140(69.1%) | 9(4.4%) | 1 | 1 |
| Attitude | ||||
| Favorable | 160(78.4%) | 26(12.7%) | [COR: 0.65(3.6-18.0] | [AOR: 0.86(1.1-6.0)] |
| Unfavorable | 13(6.4%) | 5(2.5%) | 1 | 1 |
| Monitor BGL | ||||
| yes | 46(22.5%) | 6(2.9%) | [COR: 0.44(1.6-20.0] | [AOR: 0.5(0.9-17.0)] |
| no | 140(68.6%) | 12(5.9%) | 1 | 1 |
The current study was undertaken in Debra Tabor comprehensive specialized referral hospital and the prevalence of self-reported hypoglycemia was 88.7% (95%, CI 83.8-92.6). Of the overall study participants, 93.1% (190) were aware of hypoglycemia self as well as by relatives regarding its treatment.
All patients with type 1 and type 2 DM were undergoing regular treatment and follow-up was consented before proceeding with interviewing. The prevalence of hypoglycemia was significantly associated with occupation [AOR: 4.0 (1.86-9.35)], higher educational status [AOR: 2.1 (1.9-13.1)], diabetic duration < 1 [AOR: 0.8 (1.3-9.28)], good knowledge [AOR: 0.9 (1.09-11.0)] and favorable attitude [AOR: 0.86 (1.1-6.0)].
However, the findings of the current study were 30 times higher than a similar study conducted in Jimma Medical Center and Ethiopia with the prevalence rate of hypoglycemia (at 3.3%) and (70.8%) respectively. The higher prevalence of hypoglycemia in the current study may be due to the poor attitude and practice of the respondents regarding measuring blood glucose levels [27,28].
Similarly, the findings of the current study were higher when compared with the study conducted in Ethiopia revealing that the prevalence of hypoglycemia was (14%) however the glycemic control was higher in a similar study conducted in Sudan among type 2 diabetic patients 70.5% when compared it with the current study was higher with the prevalence of hypoglycemia among the two studies [18,24].
Despite the higher prevalence of hypoglycemia in the current study, though the findings were lower when compared with the study conducted from 9 countries, the report of hypoglycemic events was 97.4% however the findings were consistent with the findings of the prospective cohort study with the prevalence of hypoglycemic state of revealed that 91.7% [28-30].
Regarding factors associated with hypoglycemia, the findings of the current study were not consistent findings with other studies but the findings Bivariable were consistent with the multivariable findings from a similar study conducted in Ethiopia [31,32].
Since DM is a chronic and debilitating pose with different complications it needs adequate knowledge for proper management and prevent complications such as hypoglycemia. The current study found that the knowledge level of the patients was good which was 81.9% (95%, CI, 76-86.8).
The findings of the current study were in line with a similar study conducted in Ethiopia with the knowledge of the respondents. The similarity of the findings may be due to similarities in the study setup, socio-demographic characteristics, and study design (77.5%) [25].
The knowledge level of the respondents was when compared with the same study conducted in Ethiopia with the level of knowledge (65.8%) and (31.3%) respectively, the higher level of knowledge may be due to awareness creation through proper counseling and health education by the health care providers [33].
However, the study findings were found to be consistent with a similar study conducted in an African country Nigeria with the findings showed that 78.96% of participants had good knowledge of [34].
The majority of the study findings were lower when compared with the current study for instance the study conducted in Africa revealed that 50% of the respondents have good knowledge regarding controlling hypoglycemia [35].
Still, the knowledge level of diabetic patients concerning hypoglycemia was 66.1% followed by 80% of the patients knowing that they must consume some sweets or chocolates and these findings revealed that almost the findings of the current study are higher in African countries including Ethiopia and India [8].
We found that more than two-thirds 73% (95% CI, 66.7-78.9) of the participants had good or poor practice in hypoglycemia prevention. This finding is lower than the study conducted in Addis Ababa and Gondar revealed that (55.4%) of study participants have fair practice to have the optimum level of glycemic agate however lower when compared in patients’ skill assessments, 94.6% correctly showed injection sites, 70% indicated injection site rotations, and 60.75% practiced injection site rotations [36,37].
However, the current study findings are almost nearly too consistent when compared with the study conducted in India which revealed that the practice of diabetes regarding hypoglycemic prevention practice of T1DM patients was found, 63.2%. This similarity may be because there is an increasing public awareness about their health status due to civilization and an increase in media coverage. The other possible reason might be differences in study participants and the study setup [26,38].
The current study also assesses the attitude of respondents regarding hypoglycemia in addition to the prevalence, knowledge, and practice of patients regarding hypoglycemia. Unfortunately the attitude; level of the respondents was higher than the knowledge and practice level of the respondents. The findings revealed that the favorable attitude of the respondents was 91.2% (95% CI, 86.8-94.6).
However, the findings of the current study were higher than a similar study conducted in Ethiopia which revealed that the overall attitude of the respondents was (73.1).
But also higher when compared with the study conducted on the assessment of self-care-related knowledge, attitude, practice, and associated factors among patients with diabetes revealed that 70.4% of the total patients had a good attitude towards control and reduction of hypoglycemia This difference might be due to the high accessibility of health care providers with specialty care in the current hospital and continuous attitudinal change through proper health education [39,40].
The attitude level of the respondents regarding the current study is also consistently higher than the study conducted in India with an attitude level of (48.5%). This may be due to the knowledge level supports to acquire a favorable attitude in addition to inheriting a favorable attitude [41-50].
Limitation
The first limitation is the cross-sectional nature of the study design which showed one result at a time and does not reflect any amendments of patients. Second, the finding may not be representative of all diabetes mellitus patients because the inclusion criteria were restricted to the adult population and chronic outpatient follow-up patients, which exclude admitted and critically ill patients, this under representative of those who are sick and do not regularly attend chronic ambulatory follow-up clinics. The third one is the center nature of the study and one region that may not represent all DM patients more widely.
In this study, a large number of the respondents had poor practices which are very significant in controlling hypoglycemia. However, the attitude level of the respondents despite practice and knowledge was higher. Hypoglycemia was highly prevalent among the diabetic patients treated at DTCSH. The increment in the prevalence of hypoglycemia was noted higher despite taking oral hypoglycemic agents and insulin. The prevalence of hypoglycemia in all forms of diabetes mellitus patients was also dramatically increasing as evidenced by this study which also implies that there is poor provision of diabetes education regarding self-blood glucose monitoring, adherence to medication, feeding styles, and other lifestyle habits like drinking, smoking, and chewing chat.
Recommendation
The following recommendations are given based on the findings of the research and conclusions.
- Health professionals working in the hospital had better provide appropriate patient advice about, monitoring, medication adherence, and self-injection as well as oral hypoglycemic agent administrations.
- Counseling and education of DM patients regarding how to reduce and avoid bad lifestyle habits like and other lifestyle habits like drinking, smoking, and chewing chat.
Health institutions should have a schedule on diabetic education along with the other ten top diseases during follow-up periods, and diabetic education specifically regarding hypoglycemia should be incorporated into the health education program of the hospitals.
Recommendation for researcher: Since the current study was conducted in a health institution better if it was conducted in a community with multicenter using mixed approaches for further investigation do as to fix a multidimensional problem in the community
Authors’ contributions
LYZ designed the study, collected and analyzed the data, interpreted the findings, and wrote the manuscript. GMA GMW and DAS were involved in the design, and data analysis, and critically revised the manuscript.
The authors are grateful to Debre-Tabor University for giving ethical approval to conduct this research and to Debre Tabor’s comprehensive and specialized Hospital. We sincerely thank the study participants for their time to participate in this study.
Declaration
Ethics approval and consent to participate: Ethical clearance was obtained from the Institutional Review Committee Debre Tabor University’s College of Medicine and Health Sciences (study protocol number-0058/2022). Then, officials at different levels in the hospitals were communicated through letters from the College of Medicine and Health Science. Before any attempt at an interview, informed verbal consent from all participants was obtained. Confidentiality of the information was secured throughout the study process. Finally, the results of the study were used only for study purposes.
Availability of data and materials: The datasets analyzed during the current study are available from the corresponding author upon reasonable request.
- Kenny C. When hypoglycemia is not obvious: diagnosing and treating under-recognized and undisclosed hypoglycemia. Prim Care Diabetes. 2014 Apr;8(1):3-11. doi: 10.1016/j.pcd.2013.09.002. Epub 2013 Oct 5. PMID: 24100231.
- Rozance PJ, Wolfsdorf JI. Hypoglycemia in the Newborn. Pediatr Clin North Am. 2019 Apr;66(2):333-342. doi: 10.1016/j.pcl.2018.12.004. Epub 2019 Feb 1. PMID: 30819340.
- Laillou A, Prak S, de Groot R, Whitney S, Conkle J, Horton L, Un SO, Dijkhuizen MA, Wieringa FT. Optimal screening of children with acute malnutrition requires a change in current WHO guidelines as MUAC and WHZ identify different patient groups. PLoS One. 2014 Jul 1;9(7):e101159. doi: 10.1371/journal.pone.0101159. PMID: 24983995; PMCID: PMC4077752.
- Garber AJ, Abrahamson MJ, Barzilay JI, Blonde L, Bloomgarden ZT, Bush MA, Dagogo-Jack S, DeFronzo RA, Einhorn D, Fonseca VA, Garber JR, Garvey WT, Grunberger G, Handelsman Y, Henry RR, Hirsch IB, Jellinger PS, McGill JB, Mechanick JI, Rosenblit PD, Umpierrez GE; American Association of Clinical Endocrinologists (AACE); American College of Endocrinology (ACE). Consensus statement by the american association of clinical endocrinologists and american college of endocrinology on the comprehensive type 2 diabetes management algorithm--2016 executive summary. Endocr Pract. 2016 Jan;22(1):84-113. doi: 10.4158/EP151126.CS. PMID: 26731084.
- McGuire H, Longson D, Adler A, Farmer A, Lewin I; Guideline Development Group. Management of type 2 diabetes in adults: summary of updated NICE guidance. BMJ. 2016 Apr 6;353:i1575. doi: 10.1136/bmj.i1575. PMID: 27052837.
- Foos V, Varol N, Curtis BH, Boye KS, Grant D, Palmer JL, McEwan P. Economic impact of severe and non-severe hypoglycemia in patients with Type 1 and Type 2 diabetes in the United States. J Med Econ. 2015 Jun;18(6):420-32. doi: 10.3111/13696998.2015.1006730. Epub 2015 Feb 11. PMID: 25629654.
- Ratzki-Leewing A, Harris SB, Mequanint S, Reichert SM, Belle Brown J, Black JE, Ryan BL. Real-world crude incidence of hypoglycemia in adults with diabetes: Results of the InHypo-DM Study, Canada. BMJ Open Diabetes Res Care. 2018 Apr 24;6(1):e000503. doi: 10.1136/bmjdrc-2017-000503. PMID: 29713480; PMCID: PMC5922478.
- Shriraam V, Mahadevan S, Anitharani M, Jagadeesh NS, Kurup SB, Vidya TA, Seshadri KG. Knowledge of hypoglycemia and its associated factors among type 2 diabetes mellitus patients in a Tertiary Care Hospital in South India. Indian J Endocrinol Metab. 2015 May-Jun;19(3):378-82. doi: 10.4103/2230-8210.152779. PMID: 25932394; PMCID: PMC4366777.
- Seo YM, Hahm JR, Kim TK, Choi WH. Factors affecting fatigue in patients with type II diabetes mellitus in Korea. Asian Nurs Res (Korean Soc Nurs Sci). 2015 Mar;9(1):60-4. doi: 10.1016/j.anr.2014.09.004. Epub 2015 Feb 18. Erratum in: Asian Nurs Res (Korean Soc Nurs Sci). 2015 Jun;9(2):176. Hahm, Jong-Ryeal [corrected to Hahm, Jong Ryeal]. PMID: 25829212.
- Fritschi C, Quinn L. Fatigue in patients with diabetes: a review. J Psychosom Res. 2010 Jul;69(1):33-41. doi: 10.1016/j.jpsychores.2010.01.021. Epub 2010 Mar 23. PMID: 20630261; PMCID: PMC2905388.
- Drivsholm T, de Fine Olivarius N, Nielsen AB, Siersma V. Symptoms, signs and complications in newly diagnosed type 2 diabetic patients, and their relationship to glycaemia, blood pressure and weight. Diabetologia. 2005 Feb;48(2):210-4. doi: 10.1007/s00125-004-1625-y. Epub 2005 Jan 14. PMID: 15650820.
- Lee AK, Lee CJ, Huang ES, Sharrett AR, Coresh J, Selvin E. Risk Factors for Severe Hypoglycemia in Black and White Adults With Diabetes: The Atherosclerosis Risk in Communities (ARIC) Study. Diabetes Care. 2017 Dec;40(12):1661-1667. doi: 10.2337/dc17-0819. Epub 2017 Sep 19. PMID: 28928117; PMCID: PMC5711330.
- Saedi E, Gheini MR, Faiz F, Arami MA. Diabetes mellitus and cognitive impairments. World J Diabetes. 2016 Sep 15;7(17):412-22. doi: 10.4239/wjd.v7.i17.412. PMID: 27660698; PMCID: PMC5027005.
- Pistrosch F, Ganz X, Bornstein SR, Birkenfeld AL, Henkel E, Hanefeld M. Risk of and risk factors for hypoglycemia and associated arrhythmias in patients with type 2 diabetes and cardiovascular disease: a cohort study under real-world conditions. Acta Diabetol. 2015 Oct;52(5):889-95. doi: 10.1007/s00592-015-0727-y. Epub 2015 Mar 10. PMID: 25749806.
- Yanai H, Adachi H, Katsuyama H, Moriyama S, Hamasaki H, Sako A. Causative anti-diabetic drugs and the underlying clinical factors for hypoglycemia in patients with diabetes. World J Diabetes. 2015 Feb 15;6(1):30-6. doi: 10.4239/wjd.v6.i1.30. PMID: 25685276; PMCID: PMC4317315.
- Takeishi S, Mori A, Hachiya H, Yumura T, Ito S, Shibuya T, Hayashi S, Fushimi N, Ohashi N, Kawai H. Hypoglycemia and glycemic variability are associated with mortality in non-intensive care unit hospitalized infectious disease patients with diabetes mellitus. J Diabetes Investig. 2016 May;7(3):429-35. doi: 10.1111/jdi.12436. Epub 2015 Nov 17. PMID: 27330731; PMCID: PMC4847899.
- Aynalem SB, Zeleke AJ. Prevalence of Diabetes Mellitus and Its Risk Factors among Individuals Aged 15 Years and Above in Mizan-Aman Town, Southwest Ethiopia, 2016: A Cross Sectional Study. Int J Endocrinol. 2018 Apr 26;2018:9317987. doi: 10.1155/2018/9317987. PMID: 29853887; PMCID: PMC5944196.
- Ibrahim SMM. Assessment of Glycemic Control and its Associated Factors among Type 2 Diabetes Mellitus Patients in Abusunoon Health Center, Greater Wad Medani Locality, Gezira State, Sudan. 2017.
- International Hypoglycaemia Study Group. Minimizing Hypoglycemia in Diabetes. Diabetes Care. 2015 Aug;38(8):1583-91. doi: 10.2337/dc15-0279. PMID: 26207052.
- Mehta HB, Mehta V, Goodwin JS. Association of Hypoglycemia With Subsequent Dementia in Older Patients With Type 2 Diabetes Mellitus. J Gerontol A Biol Sci Med Sci. 2017 Aug 1;72(8):1110-1116. doi: 10.1093/gerona/glw217. Erratum in: J Gerontol A Biol Sci Med Sci. 2019 Apr 23;74(5):750. PMID: 27784724; PMCID: PMC5861972.
- Giorda CB, Ozzello A, Gentile S, Aglialoro A, Chiambretti A, Baccetti F, Gentile FM, Lucisano G, Nicolucci A, Rossi MC; HYPOS-1 Study Group of AMD. Incidence and risk factors for severe and symptomatic hypoglycemia in type 1 diabetes. Results of the HYPOS-1 study. Acta Diabetol. 2015 Oct;52(5):845-53. doi: 10.1007/s00592-015-0713-4. Epub 2015 Feb 12. PMID: 25670242.
- Cobo A, Vázquez LA, Reviriego J, Rodríguez-Mañas L. Impact of frailty in older patients with diabetes mellitus: An overview. Endocrinol Nutr. 2016 Jun-Jul;63(6):291-303. English, Spanish. doi: 10.1016/j.endonu.2016.01.004. Epub 2016 Mar 9. PMID: 26971016.
- Weinstock RS, DuBose SN, Bergenstal RM, Chaytor NS, Peterson C, Olson BA, Munshi MN, Perrin AJ, Miller KM, Beck RW, Liljenquist DR, Aleppo G, Buse JB, Kruger D, Bhargava A, Goland RS, Edelen RC, Pratley RE, Peters AL, Rodriguez H, Ahmann AJ, Lock JP, Garg SK, Rickels MR, Hirsch IB; T1D Exchange Severe Hypoglycemia in Older Adults With Type 1 Diabetes Study Group. Risk Factors Associated With Severe Hypoglycemia in Older Adults With Type 1 Diabetes. Diabetes Care. 2016 Apr;39(4):603-10. doi: 10.2337/dc15-1426. Epub 2015 Dec 17. PMID: 26681721.
- Bedaso A, Oltaye Z, Geja E, Ayalew M. Diabetic ketoacidosis among adult patients with diabetes mellitus admitted to emergency unit of Hawassa university comprehensive specialized hospital. BMC Res Notes. 2019 Mar 14;12(1):137. doi: 10.1186/s13104-019-4186-3. PMID: 30871605; PMCID: PMC6419397.
- Muche EA, Mekonen BT. Hypoglycemia prevention practice and its associated factors among diabetes patients at university teaching hospital in Ethiopia: Cross-sectional study. PLoS One. 2020 Aug 21;15(8):e0238094. doi: 10.1371/journal.pone.0238094. PMID: 32822414; PMCID: PMC7446928.
- Gebremichael G, Zemichael T. Hypoglycemia Prevention Practice and Associated Factors Among Patients with Diabetes Mellitus Following at Public Hospitals of Central Zone, Tigray, Ethiopia, 2018. 2019.
- Negera GZ, Weldegebriel B, Fekadu G. Acute Complications of Diabetes and its Predictors among Adult Diabetic Patients at Jimma Medical Center, Southwest Ethiopia. Diabetes Metab Syndr Obes. 2020 Apr 20;13:1237-1242. doi: 10.2147/DMSO.S249163. PMID: 32368116; PMCID: PMC7182448.
- Emral R, Pathan F, Cortés CAY, El-Hefnawy MH, Goh SY, Gómez AM, Murphy A, Abusnana S, Rudijanto A, Jain A, Ma Z, Mirasol R; IO HAT Investigator Group. Self-reported hypoglycemia in insulin-treated patients with diabetes: Results from an international survey on 7289 patients from nine countries. Diabetes Res Clin Pract. 2017 Dec;134:17-28. doi: 10.1016/j.diabres.2017.07.031. Epub 2017 Aug 9. PMID: 28951336.
- Lee CJ, Wood GC, Lazo M, Brown TT, Clark JM, Still C, Benotti P. Risk of post-gastric bypass surgery hypoglycemia in nondiabetic individuals: A single center experience. Obesity (Silver Spring). 2016 Jun;24(6):1342-8. doi: 10.1002/oby.21479. PMID: 27225597; PMCID: PMC4919116.
- Lamounier RN, Geloneze B, Leite SO, Montenegro R Jr, Zajdenverg L, Fernandes M, de Oliveira Griciunas F, Ermetice MN, Chacra AR; HAT Brazil study group. Hypoglycemia incidence and awareness among insulin-treated patients with diabetes: the HAT study in Brazil. Diabetol Metab Syndr. 2018 Nov 21;10:83. doi: 10.1186/s13098-018-0379-5. PMID: 30479669; PMCID: PMC6249957.
- Nigussie S, Birhan N, Amare F, Mengistu G, Adem F, Abegaz TM. Rate of glycemic control and associated factors among type two diabetes mellitus patients in Ethiopia: A cross sectional study. PLoS One. 2021 May 11;16(5):e0251506. doi: 10.1371/journal.pone.0251506. PMID: 33974654; PMCID: PMC8112661.
- Muche EA, Mekonen BT. Hypoglycemia prevention practice and its associated factors among diabetes patients at university teaching hospital in Ethiopia: Cross-sectional study. PLoS One. 2020 Aug 21;15(8):e0238094. doi: 10.1371/journal.pone.0238094. PMID: 32822414; PMCID: PMC7446928.
- Gebremichael GB, Zemichael TM. Hypoglycemia Prevention Practice and Associated Factors Among Diabetic Mellitus Patients on Follow-up at Public Hospitals of Central Zone, Tigray, Ethiopia, 2018. 2019.
- Hamoudi NM, Al Ayoubi ID, Vanama J, Yahaya H, Usman UF. Assessment of Knowledge and Awareness of Diabetic and Non-Diabetic Population Towards Diabetes Mellitus in Kaduna, Nigeria. Journal of Advanced Scientific Research. 2012; 3.
- Ejegi A, Ross AJ, Naidoo K. Knowledge of symptoms and self-management of hypoglycaemia amongst patients attending a diabetic clinic at a regional hospital in KwaZulu-Natal. Afr J Prim Health Care Fam Med. 2016 Jun 17;8(1):e1-6. doi: 10.4102/phcfm.v8i1.906. PMID: 27380786; PMCID: PMC4926716.
- Bonger Z, Shiferaw S, Tariku EZ. Adherence to diabetic self-care practices and its associated factors among patients with type 2 diabetes in Addis Ababa, Ethiopia. Patient Prefer Adherence. 2018 Jun 6;12:963-970. doi: 10.2147/PPA.S156043. PMID: 29922042; PMCID: PMC5995298.
- Netere AK, Ashete E, Gebreyohannes EA, Belachew SA. Evaluations of knowledge, skills and practices of insulin storage and injection handling techniques of diabetic patients in Ethiopian primary hospitals. BMC Public Health. 2020 Oct 12;20(1):1537. doi: 10.1186/s12889-020-09622-4. PMID: 33046046; PMCID: PMC7552567.
- Bhutani G, Kalra S, Lamba S, Verma PK, Saini R, Grewal M. Effect of diabetic education on the knowledge, attitude and practices of diabetic patients towards prevention of hypoglycemia. Indian J Endocrinol Metab. 2015 May-Jun;19(3):383-6. doi: 10.4103/2230-8210.152781. PMID: 25932395; PMCID: PMC4366778.
- Niguse H, Belay G, Fisseha G, Desale T, Gebremedhn G. Self-care related knowledge, attitude, practice and associated factors among patients with diabetes in Ayder Comprehensive Specialized Hospital, North Ethiopia. BMC Res Notes. 2019 Jan 18;12(1):34. doi: 10.1186/s13104-019-4072-z. PMID: 30658687; PMCID: PMC6339268.
- Khunti K, Alsifri S, Aronson R, Cigrovski Berković M, Enters-Weijnen C, Forsén T, Galstyan G, Geelhoed-Duijvestijn P, Goldfracht M, Gydesen H, Kapur R, Lalic N, Ludvik B, Moberg E, Pedersen-Bjergaard U, Ramachandran A; HAT Investigator Group. Rates and predictors of hypoglycaemia in 27 585 people from 24 countries with insulin-treated type 1 and type 2 diabetes: the global HAT study. Diabetes Obes Metab. 2016 Sep;18(9):907-15. doi: 10.1111/dom.12689. Epub 2016 Jun 20. PMID: 27161418; PMCID: PMC5031206.
- Gebremichael GB, Mariye Zemicheal T. Hypoglycemia Prevention Practice and Associated Factors among Diabetic Patients on Follow-Up at Public Hospitals of Central Zone, Tigray, Ethiopia, 2018. Int J Endocrinol. 2020 Mar 13;2020:8743531. doi: 10.1155/2020/8743531. PMID: 32256577; PMCID: PMC7093907.
- Almalki MH, Hussen I, Khan SA, Almaghamsi A, Alshahrani F. Assessment of Ramadan Education and Knowledge Among Diabetic Patients. Clin Med Insights Endocrinol Diabetes. 2018 Jan 10;11:1179551417751611. doi: 10.1177/1179551417751611. PMID: 29348712; PMCID: PMC5768264.
- Das Choudhury S, Das SK, Hazra A. Survey of knowledge-attitude-practice concerning insulin use in adult diabetic patients in eastern India. Indian J Pharmacol. 2014 Jul-Aug;46(4):425-9. doi: 10.4103/0253-7613.135957. PMID: 25097283; PMCID: PMC4118538.
- DiMeglio LA, Evans-Molina C, Oram RA. Type 1 diabetes. Lancet. 2018 Jun 16;391(10138):2449-2462. doi: 10.1016/S0140-6736(18)31320-5. PMID: 29916386; PMCID: PMC6661119.
- Dømgaard M, Bagger M, Rhee NA, Burton CM, Thorsteinsson B. Individual and societal consequences of hypoglycemia: A cross-sectional survey. Postgrad Med. 2015 Jun;127(5):438-45. doi: 10.1080/00325481.2015.1045815. Epub 2015 May 14. PMID: 25971530.
- McGill DE, Levitsky LL. Management of Hypoglycemia in Children and Adolescents with Type 1 Diabetes Mellitus. Curr Diab Rep. 2016 Sep;16(9):88. doi: 10.1007/s11892-016-0771-1. PMID: 27515311.
- Pal R, Yadav U, Grover S, Saboo B, Verma A, Bhadada SK. Knowledge, attitudes and practices towards COVID-19 among young adults with Type 1 Diabetes Mellitus amid the nationwide lockdown in India: A cross-sectional survey. Diabetes Res Clin Pract. 2020 Aug;166:108344. doi: 10.1016/j.diabres.2020.108344. Epub 2020 Jul 22. PMID: 32710997; PMCID: PMC7375303.
- Pedersen-Bjergaard U, Thorsteinsson B. Reporting Severe Hypoglycemia in Type 1 Diabetes: Facts and Pitfalls. Curr Diab Rep. 2017 Oct 28;17(12):131. doi: 10.1007/s11892-017-0965-1. PMID: 29080929.
- Samya V, Shriraam V, Jasmine A, Akila GV, Anitha Rani M, Durai V, Gayathri T, Mahadevan S. Prevalence of Hypoglycemia Among Patients With Type 2 Diabetes Mellitus in a Rural Health Center in South India. J Prim Care Community Health. 2019 Jan-Dec;10:2150132719880638. doi: 10.1177/2150132719880638. PMID: 31631765; PMCID: PMC6804359.
- Venkataraman A, Kamath L, Shankar S. Knowledge, Attitude and Practice of Insulin Use of Diabetic Patients in India. medical care. 2020; 5: 6.