More Information
Submitted: May 15, 2025 | Approved: May 21, 2025 | Published: May 22, 2025
How to cite this article: Hamid S, Sheikh AH, Amreen. Unveiling Healthcare Disparities: Social Exclusion and Public Health Challenges in Rural Ganderbal, Kashmir. J Community Med Health Solut. 2025; 6(1): 039-047.
Available from: https://dx.doi.org/10.29328/journal.jcmhs.1001056
DOI: 10.29328/journal.jcmhs.1001056
Copyright license: © 2025 Hamid S, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Public health; Infrastructure; Accessibility; Affordability; Rural-urban disparities
Unveiling Healthcare Disparities: Social Exclusion and Public Health Challenges in Rural Ganderbal, Kashmir
Snober Hamid*, Aasif Hussain Sheikh and Amreen
Department of Sociology, University of Kashmir, India
*Address for Correspondence: Snober Hamid, Department of Sociology, University of Kashmir, India, Email: [email protected]
This study explores the dynamics of social exclusion in healthcare settings within the rural Ganderbal district of Kashmir, focusing on the availability of health facilities and the health-seeking behaviors of socially disadvantaged populations. Through a mixed-methods approach, combining quantitative data from interviews and qualitative insights from observation, the research reveals significant disparities in healthcare access between rural and urban areas. Key findings indicate that rural residents face exclusion due to a scarcity of hospitals, unavailability of 24-hour medical staff, inadequate infrastructure, staffing shortages, and systemic biases, compounded by environmental and occupational challenges. Communicable diseases predominate, with majority of respondents affected, and traditional healers and medical shops serve as primary care sources over formal institutions like government hospitals. Socio-economic factors, including low literacy, reliance on agriculture, and poverty, exacerbate these issues. The study highlights higher infant mortality and malnutrition rates in rural areas compared to urban centers, underscoring the need for attitudinal shifts among healthcare providers and systemic improvements in infrastructure and policy to enhance health equity. By addressing an underexplored gap in rural health research in India, this work aims to inform strategies for inclusive healthcare delivery, potentially yielding broader societal benefits through improved well-being and demographic dividends.
Social exclusion refers to the disadvantages faced by individuals or groups who are marginalized from mainstream society and unable to fully participate in normal life [1]. Originating in 1970s France, the term highlighted the plight of citizens excluded from state welfare [2]. Since the 1990s, the European Commission integrated “social exclusion” alongside “poverty” in policy discourse, culminating in the 2010 European Year for Combating Poverty and Social Exclusion [3]. Social exclusion extends beyond income-based poverty. As Atkinson [4] noted, it includes barriers to participation, access, and opportunity. The UK’s Department for International Development (DFID, 2005) defines it as a process of persistent disadvantage due to factors like caste, ethnicity, gender, disability, or geographic location.
This exclusion has direct health implications. It limits access to services, reinforces poverty, and increases vulnerability to illness [5]. In rural areas, this is worsened by poor infrastructure and isolation, affecting groups like women, the elderly, and minorities [6]. In India, rural healthcare faces both supply-side issues—like a shortage of staff—and demand-side challenges, including low health awareness and reliance on traditional practices [7]. These dynamics create a cycle of poor health outcomes, highlighting the need for inclusive health strategies [8]. In the specific context of India, the rural-urban health divide is stark, with rural areas lagging in key indicators such as life expectancy, maternal health, and child nutrition (Patel, et al. 2015). National surveys like the National Family Health Survey-4 (NFHS-4) reveal that rural populations face higher rates of communicable diseases and lower immunization coverage, often due to inadequate primary healthcare infrastructure [9]. Moreover, socio-cultural factors, including caste hierarchies and gender norms, further entrench exclusion, limiting access to care for marginalized groups [10]. In Kashmir, these challenges are intensified by the region’s geopolitical instability and climatic extremes, which disrupt healthcare delivery and exacerbate reliance on informal systems [11]. Despite initiatives like the National Rural Health Mission (NRHM), gaps in implementation persist, leaving rural communities underserved and understudied [12]. This study builds on these insights by focusing on Ganderbal, offering a lens into how local conditions shape the broader narrative of exclusion and health in rural India. Further rural children are 77% more probably to be malnourished or under height as per their age; 56% of rural South Africans reside 5 km from a health service; and 75% of South Africa’s poor people live in rural regions [13].
Even in societies where most people reside in rural areas, the resources are concentrated in the cities. All countries have complications with transportation and communication, and they all face the difficulty of deficiency of doctors and other health professionals in rural and remote areas [14]. In several developed nations, there has been a noticeable reduction in financial and infrastructural support for healthcare services in rural and remote regions. This decline coincides with transformations in key rural sectors like agriculture, mining, fishing, and forestry, alongside broader social and economic shifts that contribute to what is often termed “the rural decline” [15]. Concurrently, many rural and remote communities bear the burdens of global changes without experiencing commensurate advantages [16].
All of these concerns are emphasized in the background of repeatedly severe shortages of doctors, nurses, and other health professionals in rural and remote communities [17]. Rural health care services need adequate numbers of doctors and other health professionals who have the required expertise to work efficiently and contentedly in these areas. The sustainability of these services is reliant on sufficient health service infrastructure and accessibility of specialist support. World Health Organization (WHO) report “A Universal Truth: No Health without a Workforce” was arranged for the Third Global Forum on Human Resources for Health held in November 2013 in Recife, Brazil. This report highlighted that there is a shortage of health care professionals all over the world, which is particularly prominent in rural areas of developing or low-income countries [18]. Even though the shortage of health professionals is present globally, nowhere is this shortfall, number-wise, and skill-wise, more critical than in rural areas. In every nation, the health condition of rural inhabitants is more miserable than that of their urban counterparts [19].
Evaluating healthcare disparities, infrastructure, and opportunities for improvement in Ganderbal District
This section assesses the disparities in healthcare access, infrastructure deficits, and policy interventions in Ganderbal district, drawing on data from the 2011 Census of India, the 2017 Rural Health Statistics Report, and secondary literature to identify gaps and propose avenues for enhancement. Among the four Community Development (C.D.) blocks in the district, Lar exhibits the highest availability of medical facilities, serving 82.35% (14 out of 17) of its villages, followed by Kangan with 74.36% (29 out of 39) coverage. In contrast, Ganderbal and Wakura trail significantly, with facilities accessible to only 52.17% (12 out of 23) and 50% (17 out of 34) of their villages, respectively (Census of India, 2011). This uneven distribution leaves approximately 6 villages in Lar, 10 in Ganderbal, and 17 in Kangan without healthcare facilities, compelling residents to travel to neighboring areas for even minor ailments, thus intensifying access challenges.
The 2017 Rural Health Statistics Report by the Union Ministry of Health and Family Welfare [20] further illuminates the dire state of healthcare infrastructure in Jammu and Kashmir (J&K) [21], particularly in peripheral regions like Ganderbal. Of the 84 Community Health Centers (CHCs) operational in J&K, only 45 provide staff quarters, and just 29 have resident doctors. Moreover, only 23 CHCs are staffed with all four essential specialists—physician, pediatrician, gynecologist, and surgeon—while 17 lack functional operating theaters. At the Primary Health Center (PHC) level, approximately 20% of the 637 facilities in J&K operate without electricity or regular water supply, and 58% (375) lack ambulance services. Sub-centers (SCs) face even graver shortages: 72.6% of the 2,967 SCs in J&K lack regular water supply, 62.7% are without electricity, and 29.3% are inaccessible by motorable roads. Additionally, only 924 SCs operate from government buildings, while 2,043 are in rented spaces, with 151 still under construction. Basic amenities are similarly deficient: 87% of SCs lack staff toilets, 92% (2,743) have no separate male/female toilets, and at the CHC level, 40% (34 out of 84) lack gender-separated facilities, with 29% (24) missing staff toilets altogether [22]. These statistics highlight a systemic pattern of healthcare asymmetry in rural Ganderbal, marked by inadequate staffing, poor infrastructure, and limited service availability, all of which compromise patient care and restrict treatment options, especially for severe cases.
Aim of the study
- To investigate the prevalence of health care facilities among socially disadvantaged people in Ganderbal district
- To examine the patterns of illness and the associated behaviors related to seeking medical care.
Study design
This study employed a mixed-methods research design, integrating both descriptive and exploratory approaches to investigate healthcare access and social exclusion in rural Ganderbal district, Kashmir. The descriptive component focused on outlining socio-economic characteristics, morbidity patterns, and treatment-seeking behaviors among respondents, while the exploratory component examined underlying factors contributing to health-based exclusion and discrimination. A bi-polar strategy was adopted, combining quantitative and qualitative techniques to provide a comprehensive understanding of the research problem.
Research strategies
The study followed inductive and abductive research logics to address the “what” and “why” of rural healthcare exclusion. Quantitative data were collected through semi-structured interview schedules, enabling systematic gathering of first-hand information from participants across sampled villages. Qualitative data were obtained via observational methods, allowing researchers to capture contextual nuances and lived experiences related to healthcare access and utilization. This dual approach ensured triangulation of findings, enhancing the reliability and depth of the analysis.
Sampling
A combination of purposive and convenience sampling techniques was utilized to align with the study’s objectives. The research deliberately targeted rural villages in Ganderbal district lacking healthcare facilities, focusing one medical block of district Ganderbal i.e., block Ganderbal. Within this block, two villages Ganderbal (urban) and Shearpathari (rural) were randomly selected to ensure representativeness. A total of 200 respondents were interviewed, chosen based on accessibility and willingness to participate, to explore morbidity patterns, health-seeking behaviors, and medication use. The sample size was determined to balance feasibility with statistical robustness given the study’s resource constraints.
Study population and setting
The universe of the study encompassed Ganderbal district, located in the Kashmir division of Jammu and Kashmir, India. Established as a distinct district on April 1, 2007, Ganderbal comprises six tehsils (Ganderbal, Lar, Kangan, Tullamulla, Gund, and Wakura) and nine blocks (Ganderbal, Lar, Kangan, Wakura, Gund, Shearpathri, Phaag, Manigam, and Batwina). The district’s healthcare infrastructure includes two sub-district hospitals (Ganderbal and Kangan), one trauma hospital (Kangan), 29 primary health centers, and 84 sub-centers, as per available data [22]. Villages without healthcare facilities were prioritized to assess the extent of rural exclusion.
Data collection
Quantitative data were gathered using a semi-structured interview schedule administered to the 200 respondents. This tool captured demographic details (e.g., gender, age, income, education), morbidity patterns, healthcare-seeking behaviors, and preferences for treatment modalities (e.g., allopathy, traditional medicine). Interviews were conducted in person across selected villages to ensure direct engagement with participants. Qualitative data were collected through unstructured observations in the field, focusing on healthcare facility conditions, patient interactions, and environmental factors influencing access. Secondary data, including statistical figures on healthcare infrastructure, were sourced from the District Census Handbook [22] and the Rural Health Statistics Report (2017) to substantiate field findings.
Data analysis
Quantitative data from the interview schedules were tabulated and analyzed using descriptive statistics (e.g., frequencies, percentages) to identify patterns in socio-economic profiles, disease prevalence, and healthcare utilization. Tables and bar charts were generated to visually represent key findings, such as the distribution of healthcare facilities and treatment preferences. Qualitative data from observations were analyzed thematically, with narratives and participant quotes coded to highlight recurring issues like infrastructure deficits, staffing shortages, and discrimination. Secondary data were synthesized to provide a comparative context and validate primary findings. The integration of these analyses enabled a holistic assessment of healthcare asymmetries in the district.
Ethical considerations
The study adhered to ethical research principles, ensuring informed consent from all participants. Respondents were briefed about the study’s purpose, and participation was voluntary, with the option to withdraw at any time. Confidentiality was maintained by anonymizing personal data in the reporting of results. No financial incentives were provided, and the research posed no physical or psychological risks to participants.
Findings of the study
Morbidity pattern and treatment seeking behaviour among the sample respondents (Table 1): The socio-economic and demographic profile of the respondents reveals several key insights. The majority of respondents (83.5%) are male, while only 16.5% are female. In terms of marital status, 90% are married, suggesting that marriage is a prevalent social norm. Educational attainment is generally low, with 55.5% of respondents being illiterate, 21.5% having primary education, 12% reaching the secondary level, and only 11% completing graduation. This reflects limited access to higher education, which may influence employment opportunities and economic conditions.
| Table 1: Socio-economic and Demographic Profile of the Respondents. | ||
| Socio-economic and Demographic Variables | Frequencies | Percentages |
| Gender Status | ||
| Male | 167 | 83.5 |
| Female | 33 | 16.5 |
| Total | 200 | 100.00 |
| Marital Status | ||
| Married | 180 | 90.00 |
| Unmarried | 20 | 10.00 |
| Total | 200 | 100.00 |
| Educational Status | ||
| Illiterate | 111 | 55.5 |
| Primary | 43 | 21.5 |
| Secondary | 24 | 12.00 |
| Graduation | 22 | 11.00 |
| Total | 200 | 100.00 |
Caste Groups |
||
| Sheikh (Wattal) | 80 | 40.00 |
| Kumar | 60 | 30.00 |
| Doomb | 33 | 16.5 |
| Ganie | 27 | 13.5 |
| Total | 200 | 100.00 |
| Occupation Status | ||
| Agricultural labourers | 105 | 52.5 |
| Businessmen/ Private | 13 | 6.5 |
| Govt. Employment | 20 | 10.00 |
| Total | 200 | 100.00 |
| Income Stauts(in Rs) | ||
| Below-10000 | 143 | 71.5 |
| 10001-20000 | 37 | 36.5 |
| 20001-40000 | 10 | 5.00 |
| Above-41000 | 0 | 0.00 |
| Total | 200 | 100.00 |
| Age Groups | ||
| 15-30 | 35 | 17.5 |
| 31-45 | 85 | 42.5 |
| 46-60 | 60 | 30 |
| Above 60 | 20 | 10 |
| Total | 200 | 100.00 |
| Type of Family | ||
| Joint family | 133 | 75.00 |
| Nuclear Family | 77 | 25.00 |
| Total | 200 | 100.00 |
| Type of House | ||
| Pucca | 53 | 26.5 |
| Semi Pucca | 66 | 33.00 |
| Kaccha | 81 | 40.5 |
| Total | 200 | 100.00 |
The caste composition shows that the largest group is Sheikh (Wattal) (40%), followed by Kumar (30%), Doomb (16.5%), and Ganie (13.5%), highlighting caste diversity in the community. Occupational data indicates that 52.5% of respondents are agricultural laborers, while 10% are government employees and only 6.5% are engaged in business or private jobs, pointing to a heavy reliance on agriculture for livelihood. Income distribution further underscores economic challenges, with 71.5% earning below ₹10,000 per month, 18.5% earning between ₹10,001 and ₹20,000, and only 5% falling within the ₹20,001–40,000 range. Notably, none of the respondents earn above ₹41,000, reflecting a lack of high-income earners.
Age-wise, the largest group (42.5%) falls within the 31–45 age range, followed by 30% in the 46–60 category, 17.5% in the 15–30 age group, and only 10% above 60 years, indicating that most respondents are middle-aged. Family structure analysis shows that 75% of the respondents live in joint families, while 25% belong to nuclear families, suggesting a preference for traditional family systems. Housing conditions reveal that 40.5% reside in kaccha houses, 33% in semi-pucca houses, and only 26.5% in pucca houses, further reflecting economic constraints.
Overall, the data indicates that the surveyed population faces socio-economic challenges, including low literacy rates, limited occupational diversity, and financial hardships. The predominance of agricultural laborers, low-income levels, and poor housing conditions highlight the need for targeted interventions in education, employment diversification, and housing improvement to enhance their overall living standards.
The socio-economic determinants of health play a vital role in improving health indicators and social development. The poor socio-economic background of an individual has an adverse effect on their health and well-being.
Table 2 presents the socio-economic and demographic characteristics of the respondents in relation to their illness status, healthcare-seeking behavior, and preference for different types of medication.
| Table 2: Socio-economic variable of Respondents in relation with Morbidity Pattern and Health-care Seeking Behaviour. | |||||||||||||
| Socio-economic and Demographic Variables | Level of Care | Type of Medicine | Type of Diseases | ||||||||||
| Block PHC | Govt. Hospital | Medical Shop | Private Hospital | Traditional Healer | Allopathy | Homeopathy | Ayurvedic | Unani | Others | Communicable Disease | Non-Communicable D isease | ||
| Gender | Male | 4% | 1.5% | 31.5 | 16.5% | 30% | 42% | 8% | 16.5% | 5% | 12% | 71.5% | 12% |
| Female | 5.5% | 3% | 3% | 0 | 5% | 6.5% | 2% | 0 | 0 | 8% | 13.5% | 3% | |
| Marital Status | Married | 7% | 3% | 30% | 15% | 35% | 41% | 10% | 14% | 5% | 20% | 75% | 15% |
| Unmarried | 2.5% | 1.5% | 4.5% | 1.5% | 0 | 7.5% | 0 | 2.5% | 0 | 0 | 10% | 0 | |
| Educational Status | Illiterate | 3% | 1.5% | 15% | 10% | 26% | 17.5% | 6.5% | 10% | 3.5% | 18.5% | 50% | 5.5% |
| Primary | 4% | 2.5% | 5% | 5% | 5% | 9% | 2.5% | 6.5% | 1.5% | 2% | 20% | 1.5% | |
| Secondary | 0% | 0.5% | 6% | 1.5% | 4% | 11% | 1% | 0% | 0% | 0% | 12.5% | 0.5% | |
| Graduation | 2.5% | 0% | 8.5% | 0% | 0% | 11% | 0% | 0% | 0% | 0% | 3.5% | 7.5% | |
| Occupational Status |
Agricultural labourers | 2% | 2% | 17.5% | 9.5% | 21.5% | 17% | 6.5% | 9% | 3.5% | 16.5% | 46% | 6.5% |
| Casual labour | 2% | 1.5% | 12.5% | 3% | 12% | 15% | 3.5% | 7.5% | 1.5% | 3.5% | 26% | 5% | |
| Businessmen/ Private | 3% | 0% | 1% | 2.5% | 0% | 6.5% | 0% | 0% | 0% | 0% | 5% | 1.5% | |
| Govt. Employed | 2.5% | 1% | 3.5% | 1.5% | 1.5% | 10% | 0% | 0% | 0% | 0% | 8% | 2% | |
| Income Status | Below-10000 | 4.5% | 1.5% | 22% | 11.5% | 32.5% | 32% | 4% | 16.5% | 5% | 14% | 70% | 1.5% |
| 10001-20000 | 3.5% | 1% | 7.5% | 4% | 2.5% | 9% | 3.5% | 3% | 0% | 6% | 12.5% | 6% | |
| 20001-40000 | 1.5% | 2% | 5% | 1.5% | 0% | 7.5% | 2.5% | 0% | 0% | 0% | 2.5% | 7.5% | |
| Above-41000 | 0% | 0% | 0% | 0 | 0% | 0% | 0% | 0% | 0% | 0% | 0% | 0.0 | |
| Age Groups | 15-30 | 2% | 0% | 11.5% | 5.5% | 0% | 17.5% | 0% | 0% | 0% | 0% | 17.5% | 0.0 |
| 31-45 | 3.5% | 0% | 15% | 11% | 13% | 15.5% | 4.5% | 11% | 2.5% | 9% | 37.5% | 5% | |
| 46-60 | 5% | 2% | 6% | 0% | 17% | 10.5% | 3% | 55% | 2.5% | 8.5% | 30 | 2.5% | |
| Above 60 | 0% | 2.5% | 2.5% | 0% | 5% | 5% | 2.5% | 0% | 0% | 2.5% | 2.5% | 7.5% | |
| Caste Groups | Sheikh (Wattal) | 5% | 2% | 12.5% | 8.5% | 12% | 14.5% | 3% | 9.5% | 4% | 9% | 35% | 5% |
| Kumar | 2.5% | 1.5% | 11.5% | 5% | 10% | 16.5% | 3.5% | 5% | 0% | 5% | 25% | 5% | |
| Doomb | 2% | 1% | 6.5% | 1.5% | 5.6% | 8% | 1.5% | 0% | 1% | 6% | 15% | 1.5% | |
| Ganie | 0% | 0% | 4.5% | 1.5% | 7.5% | 9.5% | 2% | 2% | 0% | 0% | 10% | 3.5% | |
| Source: Field Study | |||||||||||||
The Table shows that out of the total respondents (200), most male respondents (30%) seek treatment from traditional healers, 31% from medical shops, and 16.5% from private hospitals/clinics. It further depicts that the majority (42%) of the respondent used allopathic medicines while suffering from any diseases. It also demonstrates that the trends of communicable diseases are higher by 71% than the non-communicable disease. Hence, NCDs are also increasing.
Similarly, the table shows a significant disparity in accessing health care services and morbidity patterns between the female and male respondents. However, it shows that the female respondents primarily seek treatment from govt sources. It shows that 8% of female patients used traditional medicine, 13.5 % have communicable diseases, and 3% have non-communicable diseases.
The Table also explores the marital status of the respondents. It shows that most married respondents, 35%, have gone to traditional healers, 41% used allopathic medicines, and 75% have communicable diseases.
Moreover, it reveals that the ratio of illiterate is higher in traditional healers, private hospital, and medical shop 26%, 10%, and 15%, respectively, than literate. It also reveals that most illiterate respondents (18.5%) used traditional medicine and 50% have communicable diseases.
It shows that agriculture labourers and casual labourers have a higher ratio in communicable diseases, 46% and 26% respectively, than the other two occupations (Businessmen/ Private and govt employed). It reveals that 21.5% of agriculture labourers have chosen traditional healers for their treatment and 16.5% used various kinds of traditional medicines in which they have been satisfied. Similarly, 12% of casual labourers used to go for traditional healers, and 17% used allopathic medicines.
The table also shows the disparity in healthcare-seeking behavior and morbidity pattern in different income groups. It reveals that the majority (32.5%) of the low-income group respondents (below-10000) used traditional healers as their primary source of seeking treatment and 22% depend on the medical shops. It also explores that 32% took allopathic medicine, and 70% are suffering from communicable diseases.
Furthermore, it depicts that the Sheikh Caste (Wattal, cobbler) have the highest number of respondent who experienced the most health-based exclusion in the study area. It is empirically shown in the table that only 7% sort partial treatment in public hospitals. And the remaining 93% sort treatment from the private hospital, medical shop, and traditional healers. It further demonstrates that the trends of communicable and non-communicable diseases are higher in Sheikh (Wattal) Caste among all castes in the study area. The inclination towards utilizing allopathic medicines is higher than other sources of medicine in Sheikh Caste than other castes (Figure 1).
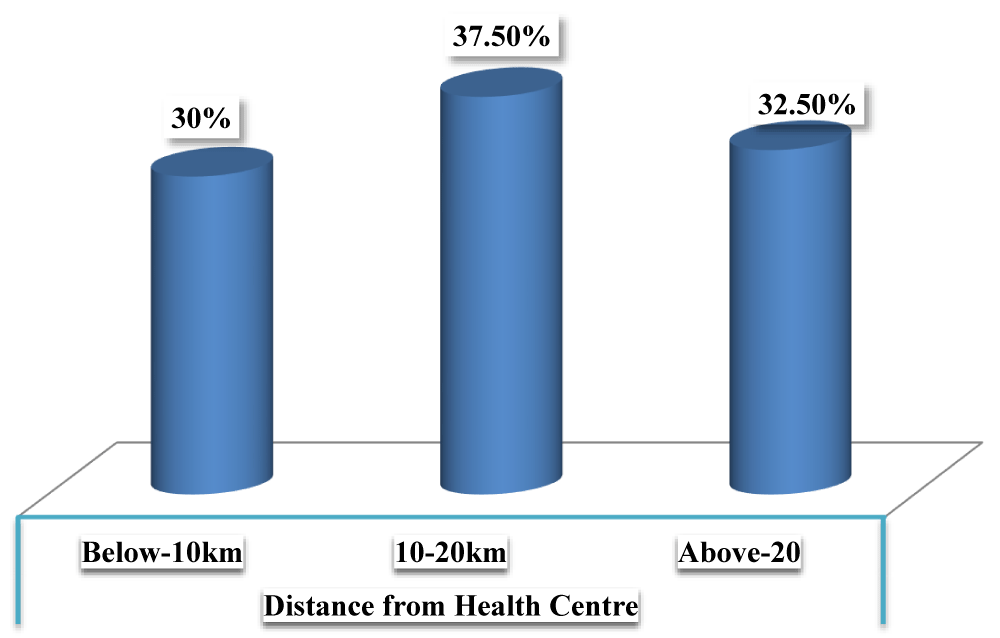
Figure 1: Percentage of respondents on the basic of distance from health center. Source: Field study.
The bar chart illustrates the distribution of respondents based on their distance from the nearest healthcare center. The highest proportion (37.5%) resides 10–20 km away, while 32.5% live more than 20 km from a health center, highlighting accessibility challenges. Only 30% of respondents are located within 10 km, indicating that a significant portion of the population faces considerable travel distances for healthcare services. These findings emphasize the need for improved healthcare accessibility, particularly for those living farther away (Figure 2).
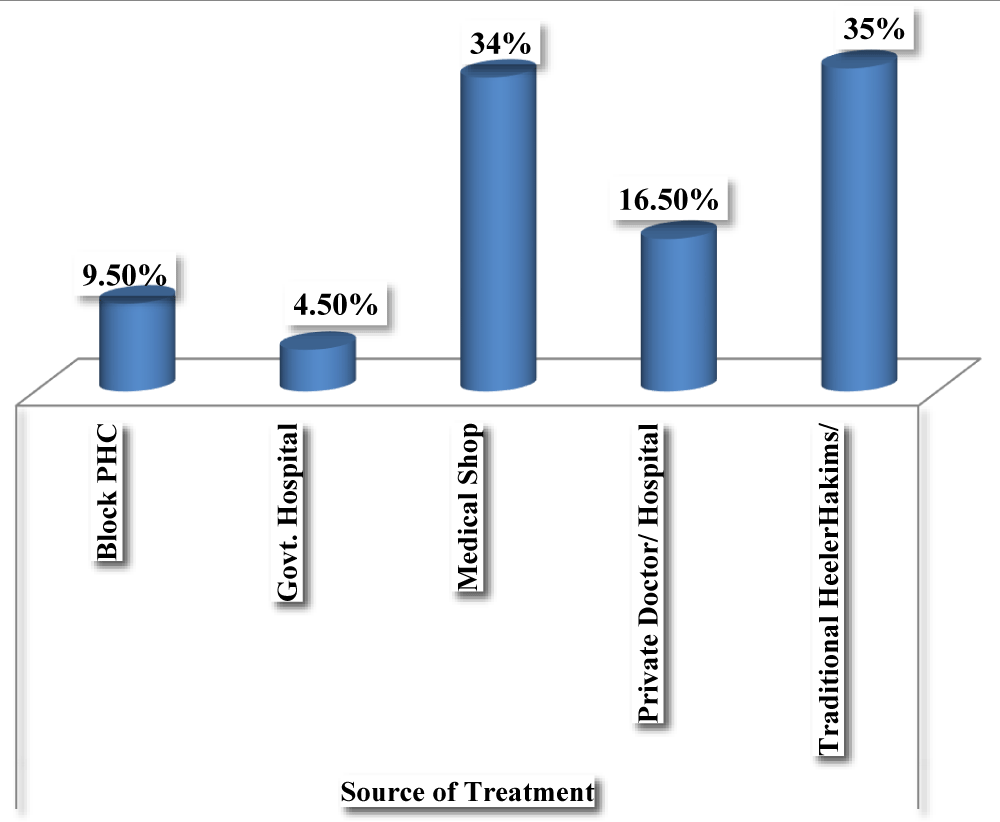
Figure 2: Source of treatment wise percentage of respondents. Source: Field study.
The bar chart represents the percentage distribution of respondents based on their preferred sources of treatment. Traditional healers (Hakims) are the most commonly sought treatment option, accounting for 35% of respondents, followed closely by medical shops at 34%. Private Doctors or hospitals are utilized by 16.5% of individuals, while only 9.5% visit Block PHCs, and a mere 4.5% seek treatment at government hospitals. The data highlights a strong reliance on traditional and informal healthcare providers over formal medical institutions.
Asymmetries in healthcare setting: narration based approach
Deficiency of hospitals: One of the major problems faced by rural people in district Ganderbal is the lack of hospitals, especially District hospitals. Far-flung villages also lack even primary health center facilities for which they have to travel long distances even for cold and cough. However, participants revealed that this creates lot of problems for them, given that they are poor.
One of the participants revealed that
“The construction of Ganderbal District Hospital, the primary healthcare facility in the region, began in 2009 with the goal of enhancing medical services for local residents. Yet, despite over a decade passing, the hospital remains incomplete, crushing the hopes of those eagerly anticipating its opening. This delay exposes the state government’s unfulfilled commitment to providing quality healthcare in remote areas and worsens the situation due to the absence of modern equipment, compelling residents to travel to Srinagar city for proper treatment, which adds a significant financial burden”.
Another participant from a tribal village said,
“Although the Ganderbal District Hospital has recently begun operations, it lacks essential equipment to function effectively. In my area, we don’t even have a basic dispensary to rely on. This absence of proper healthcare facilities forces residents to grapple with numerous challenges, including limited access to timely medical care, increased travel to distant cities like Srinagar for treatment, and the resulting financial strain. The lack of adequate infrastructure also heightens the risk of untreated illnesses, delays in emergency care, and an overall decline in community health and well-being”.
Absence of the round the clock doctors at SDHs and primary health centers
Findings further highlighted that significant challenge for residents is the lack of round-the-clock doctor availability in nearly all hospitals. People reported that despite their persistent requests, no improvements have been made. While some primary health centers in the district, particularly in remote areas, are officially designated as operating 24/7, this exists only on paper and not in reality. One resident explained, “If someone falls sick in the evening or at night, we can’t go to the nearby health center because not even a paramedic is present during those hours.
Another respondent narrated a story that highlights the plight of these rural people and the inefficiency of government in this regard “one day a man met with an accident on the highway near Barsoo area of the district. The man, who happened to be a local resident, was critically injured and directly rushed to the local hospital by people in the hospital. Neither any doctor was present there nor was an ambulance available to carry him to Soura hospital. Although one paramedic was present there, then he too was unable to help because of the non-availability of doctor”.
Certain respondents voiced their discontent, stating that these hospitals are ineffective in carrying out their role, as patients in need of urgent care endure prolonged suffering due to the lack of available doctors. They even called for the closure of these establishments, claiming they do not adequately serve the population’s healthcare requirements.
In this connection, one more participant said, “an ambulance driver of district hospital opened the door of this dispensary three years before. Since then, not a single doctor or any other staff member came here. Look over the condition of the dispensary; it has become a home for birds and animals. Its doors, walls, and windows have been damaged as no one guards it. Had it been in the city, it would have been under surveillance”.
Dearth of staff
The study also revealed that there was a dearth of staff, including doctors, nurses, and paramedics, etc., in these hospitals or health centers. “The primary health centers in our locality have been left at the clemency of a lone doctor. How can a single doctor do fairness with scores of patients who come to the hospital with an expectation to get appropriate treatment, narrated one of them?
Another participant said, “in our dispensary, there is only one lady doctor in our hospital who has not only to prescribe and provide treatment to the patients but also has to perform the work of gatekeeper, nurse, and cleric. She is always busy in maintaining records of the number of rural pregnant women, disabled people, mental illness, and chronic patients of the whole village. Tell me how she can manage OPD and all this”.
Lack of infrastructure
Respondents also reported inadequacy of infrastructure and other fundamental medical services and amenities. Few of them alleged that maximum hospitals or health centers operate in small buildings with only a few rooms since their establishment. They highlighted that besides the shortage of infrastructural crunch; the non-availability of constant electricity supply impedes patient care and adds to their misery.
Bashir Ahmad, a resident, reported that “Once I was having acute toothache and I went to the SDH hospital Kangan for dental treatment, but I was told that there is no electricity and came back when the electricity comes. It is pathetic that an SDH does not have a generator or inverter facility.”
Also, the study revealed that there is a death of beds in hospitals. Sometimes one single bed at a time is shared by two or even three patients. Furthermore, essential investigative services like ECG and USG are not present as well. “The deficiency of enough facilities and important diagnostic services compel us to go for private doctors and clinics, which is an expensive business. Although there is an X-ray unit in our local hospital, however, the technical staff members remain available for only three days per week,” lamented another local.
The respondents also stated that the non-availability of the amenities and other services had miscued the health-care system, forcing the patients to visit hospitals in Srinagar. “There should be appropriate medical equipment and staff members on hand at these health centers,” he said. “At least vital aid and medicines for small diseases should be available.” said another participant.
Natural circumstances
The winter season in Kashmir, spanning three months from December to February, plays a critical role in the health of the region’s population. There exists a strong connection between weather conditions and health outcomes. During these months, the extreme cold heightens the likelihood of illnesses, placing significant strain on healthcare facilities [23]. This surge in demand exacerbates the challenges faced by hospitals, particularly in areas already grappling with limited resources and infrastructure.
In this regard one of the respondent namely Ghulam Ahmad Sofi, an elderly man over 100 years old, shared that the most common health issues in the area include headaches, blurred vision, back pain, abdominal discomfort, limb aches, and respiratory infections, which spike significantly in winter but occur to a lesser extent in other seasons.
Neyaz Ahmad Bhat from Chattergul added that “accessing city healthcare during snowfall is both difficult and dangerous due to the absence of local medical facilities, forcing residents to rely on horses to transport patients to more developed areas”.
Another resident, Fatima Begum from a remote village, explained, “When my son fell ill with a high fever last winter, we had no choice but to wrap him in blankets and tie him to a horse for the journey. The roads were blocked, and no doctor was available nearby—it’s a risk we’re forced to take.” Similarly, Mohammad Yousuf, a father of three, recounted, “My wife suffered severe stomach pain during a snowstorm, and with no clinic in our vicinity, we struggled for hours to reach a hospital using a makeshift sled pulled by mules. The lack of basic care here endangers lives every day.” These accounts underscore the dire healthcare situation, where the absence of local services and harsh weather conditions leave residents with no option but to undertake perilous journeys for treatment.
Rural occupational structure and health
The economy of the Kashmir Valley relies heavily on traditional occupations, typically carried out within homes. Activities such as carpet weaving, mat weaving, shawl weaving, and basket-making demand long and strenuous working hours, significantly impacting the health of rural residents [24]. These labor-intensive tasks contribute to physical strain and chronic health issues, forcing many in these communities to bear substantial out-of-pocket healthcare expenses [25]. The study rectified that no aid or provision for occupational injuries was there in the industrial or working centers. There are approximately 20 handicraft training centres in the rural areas of Ganderbal, but none of them is under the coverage of health care facilities. For a minor occupational injury, they need to visit outside the rural setting, which costs their workday and wages. Therefore, they are at a double disadvantage. In this regard, some of the participants said;
Shazia Begum, a 38-year-old mother of two from a small village in the Ganderbal district, has spent over 15 years hunched over a loom, weaving intricate carpets to support her family. “We work from dawn till late at night,” she says, rubbing her aching back. “The patterns are beautiful, but the pain in my shoulders and the constant headaches are the price I pay.” The long hours of sitting in one position have left her with chronic back pain and blurred vision, yet she has no choice but to continue. Last month, when her cough worsened, she spent nearly all her savings—earned from selling a carpet—on a trip to a private clinic in the city, as the local health center had no doctor available. “We weave to survive, but the money we make goes straight to medicines and travel. What kind of life is this?” she asks her voice heavy with exhaustion.
Abdul Rahim, a 45-year-old basket maker from a remote village choudwaliwar, has woven willow mats and baskets since youth. “It sustains us but ruins my body,” he says, showing calloused hands and sore joints. Repetitive strain causes limb pain, worsened by winter respiratory issues. Last winter, unable to afford private care, he borrowed money for a horse cart to a public clinic 20 kilometers away, finding no doctor. “Our hard-earned money just goes to healthcare,” he sighs.
Rehana Bano, a 32-year-old shawl weaver from a rural village of Sonamarg, has spent years bent over her loom, her eyes straining to perfect each thread. “This work is our lifeline, but it’s stealing my sight and strength,” she whispers, her hands trembling from constant pain. The relentless task has left her with blurred vision and aching limbs, and last month, her toddler’s fever forced her to sell a shawl to afford medicine—no local clinic could help. “I wove day and night for that money, and now it’s gone. My child still coughs, and I’m breaking apart,” she says, tears welling up “Due to long working hours, we are always going through back pain, leg pain, and chest pain. But for treatment, we have neither first aid in the workshop nor in the local dispensary”.
The traditional occupations prevalent in rural Kashmir, such as basket weaving and shawl making, impose severe physical burdens on artisans, leading to chronic health conditions like joint pain, vision impairment, and respiratory issues, particularly during the harsh winter months [26]. These health challenges are compounded by the lack of accessible healthcare facilities, forcing individuals to deplete their limited earnings on out-of-pocket medical expenses or risky travel to distant hospitals [27]. For many, like Abdul Rahim and Rehana Bano, the income from their labor-intensive crafts is entirely consumed by healthcare costs, perpetuating a cycle of poverty and untreated illness [27].
The healthcare crisis in rural Ganderbal stems from a combination of socio-economic deprivation, inadequate infrastructure, and systemic neglect. The region’s healthcare facilities—84 sub-centers, only 6 maternity hospitals, and 4 allopathic dispensaries—fail to meet the needs of its widely dispersed population, particularly those in remote villages. High morbidity, especially from communicable diseases, is exacerbated by barriers to timely and effective treatment, trapping residents in a continuous cycle of illness and poverty. To address these disparities, a comprehensive strategy is required—expanding functional healthcare centers, improving staffing and medical resources, increasing awareness of government healthcare schemes, and eliminating biases among providers to ensure fair and accessible care. Without such interventions, rural communities in Ganderbal will remain excluded from adequate healthcare, falling far behind urban standards.
The healthcare system in Ganderbal is riddled with inequities that severely impact its rural population. The incomplete District Hospital, along with the absence of basic dispensaries in remote areas, forces residents to undertake long, costly, and often dangerous journeys to access medical care. A lack of round-the-clock doctors at sub-district hospitals and primary health centers renders these facilities ineffective, particularly in emergencies, as seen in cases where critically ill or injured patients are left unattended. Additionally, a severe shortage of medical staff, combined with poor infrastructure—including the lack of hospital beds, electricity, and diagnostic tools such as ECG and X-ray services—further cripples public healthcare. This forces many residents to either turn to unaffordable private care or forgo treatment altogether, worsening health outcomes and financial hardships.
Beyond inadequate infrastructure, harsh winters and an exploitative occupational structure further strain the fragile healthcare system. Rural artisans engaged in labor-intensive crafts, such as weaving and basket-making, suffer from chronic health conditions with no institutional support, compelling them to spend their meager earnings on healthcare. At the same time, natural barriers like heavy snowfall force residents to rely on rudimentary transport methods, such as horses and sleds, to reach distant medical facilities. Moreover, systemic discrimination further marginalizes vulnerable groups, as seen in Suraiya’s tragic loss due to medical negligence. These combined failures perpetuate a cycle of poverty and illness, making urgent reforms—such as improved infrastructure, increased staffing, accessible facilities, and policies addressing occupational health and discrimination—essential to achieving equitable healthcare in Ganderbal.
- Piachaud D, Bennett F, Nazroo J, Popay J. Report of task group 9: social inclusion and social mobility [Internet]. London: Institute of Health Equity; 2009. Available from: https://www.instituteofhealthequity.org/resources-reports/social-inclusion-and-social-mobility-task-group-report/task-group-9-social-inclusion-and-social-mobility-full.pdf
- Lenoir R. Les Exclus: Un Francais sur Dix. Paris: du Seuil; 1974 [cited 2025 May 21]. Available from: https://www.scirp.org/reference/referencespapers?referenceid=2282336
- Daly M. Social exclusion as concept and policy template in the European Union. Centre for European Studies Working Paper. 2006;(135). Available from: https://www.researchgate.net/publication/29998617_Social_Exclusion_as_Concept_and_Policy_Templatein_the_European_Union_CES_Working_Paper_no_135_2006
- Atkinson AB. Poverty in Europe [Internet]. Oxford: Wiley-Blackwell; 1998 [cited 2025 May 21]. Available from: https://books.google.co.in/books/about/Poverty_in_Europe.html?id=BOu_QgAACAAJ&redir_esc=y
- Burchardt T, Le Grand J, Piachaud D. Degrees of exclusion: developing a dynamic, multidimensional measure. In: Hills J, Le Grand J, Piachaud D, editors. Understanding social exclusion. Oxford: Oxford University Press; 2002. p. 30–43. Available from: https://www.scirp.org/reference/referencespapers?referenceid=2282319
- Farmer J, Muñoz SA, Threlkeld G. Theorizing rural health: a social determinants approach. Health Place. 2010 Sep;16(5):1055–62.
- Peters DH, Garg A, Bloom G, Walker DG, Brieger WR, Rahman MH. Poverty and access to health care in developing countries. Ann N Y Acad Sci. 2008 Jul;1136(1):161–71. Available from: https://doi.org/10.1196/annals.1425.011
- Commission on Social Determinants of Health (CSDH). Closing the gap in a generation: health equity through action on the social determinants of health [Internet]. Geneva: World Health Organization; 2008. Available from: https://www.who.int/publications/i/item/WHO-IER-CSDH-08.1
- International Institute for Population Sciences (IIPS). National Family Health Survey-4 (NFHS-4), 2015-16: India [Internet]. Mumbai: IIPS; 2017. Available from: https://www.dhsprogram.com/pubs/pdf/fr339/fr339.pdf
- Baru R, Acharya A, Acharya S, Kumar AKS, Nagaraj K. Inequities in access to health services in India: caste, class and region. Econ Polit Wkly. 2010 Sep 18;45(38):49–58. Available from: http://www.indiaenvironmentportal.org.in/files/Inequities%20in%20access%20to%20health%20services.pdf
- Kaul N, Chopra S. Health and conflict: A study of healthcare challenges in Jammu and Kashmir. J Peace Stud. 2019;26(3):45–60.
- Reddy KS, Patel V, Jha P, Paul VK, Kumar AKS, Dandona L. Towards achievement of universal health care in India by 2020: A call to action. Lancet. 2011 Feb 19;377(9767):760–8. Available from: https://doi.org/10.1016/s0140-6736(10)61960-5
- Boulle A. Rural health care and rural poverty inextricably linked policy in progress. Health Syst Trust Up. 1997;28:6–7.
- Strasser RP, Harvey D, Burley M. The health service needs of small rural communities. Aust J Rural Health. 1994;2(2):7–13. Available from: https://doi.org/10.1111/j.1440-1584.1994.tb00102.x
- Lawrence GA, Williams CJ. The dynamics of decline: implications for social welfare delivery in rural Australia. In: Cullen T, Dunn P, Lawrence GA, editors. Rural Health and Welfare in Australia. Wagga Wagga, NSW: Centre for Rural Welfare Research, Charles Sturt University-Riverina; 1990;38–59. Available from: https://www.nintione.com.au/resources/rao/the-dynamics-of-decline-implications-for-social-welfare-in-rural-australia/
- Birrell B, Dibden J, Wainer J. Regional Victoria: Why the Bush is Hurting [Internet]. Melbourne: Centre for Population and Urban Research, Monash University; 2000. Available from: https://www.researchgate.net/publication/237634313_Regional_Victoria_Why_the_Bush_Is_Hurting
- World Organization of Family Doctors (WONCA). Policy on Training for Rural Practice. Hong Kong: WONCA; 1995.
- Campbell J, Dussault G, Buchan J, Pozo-Martin F, Guerra AM. A Universal Truth: No Health without a Workforce [Internet]. Geneva: WHO, Global Health Workforce Alliance; 2013. Available from: https://www.who.int/publications/m/item/hrh_universal_truth
- Awofeso N. Improving health workforce recruitment and retention in rural and remote regions of Nigeria. Rural Remote Health. 2010;10(1):1319–29. Available from: https://pubmed.ncbi.nlm.nih.gov/20136347/
- Ministry of Health and Family Welfare. National Family Health Survey-4: 2015–16. Mumbai: International Institute for Population Sciences. Available from: https://www.epw.in/journal/2015/25/web-exclusives/national-family-health-survey-4.html
- Government of Jammu and Kashmir. Draft Master Plan. Gurgaon: M/S Feedback Infra Private Limited; 2013.
- Census of India. District Census Handbook Ganderbal: Village and Town Wise Primary Census Abstract (PCA). Vol. 02. New Delhi: Directorate of Census Operations; 2011.
- Ahmad S. Impact of weather on public health in Kashmir: A seasonal analysis. J Environ Health Stud. 2019;12(3):45–56.
- Sharma P. Traditional occupations and their health implications in the Kashmir Valley. Rural Dev Rev. 2021;8(4):112–25.
- Khan A, Mir R. Economic patterns and health expenditure in rural Kashmir. South Asian J Public Health. 2020;15(2):78–89.
- Hussain M. Occupational health risks in traditional Kashmiri crafts. J Rural Health Stud. 2022;19(1):23–34.
- Rather S, Qureshi N. Economic and health disparities in Kashmir’s rural workforce. Asian Public Health Rev. 2021;10(3):56–67.
- Gartner A, Gibbon R, Riley N. A profile of rural health in Wales [Internet]. Wales Centre for Health: Canolfan Lechyd Cymru; 2007 [cited 2025 May 21]. Available from: https://phw.nhs.wales/services-and-teams/observatory/data-and-analysis/ad-hoc-publications/a-profile-of-rural-health-in-wales-pdf/
- Hussain M. Rural development and health - a case study of the Ganderbal block. J Exclusion Stud [Internet]. 2012;2(1):63. Available from: http://dx.doi.org/10.5958/j.2231-4547.2.1.008
- Mukherjee S, Levesque JF. Changing inequalities in utilisation of inpatient care in rural India: Evidence from the NSS. Econ Polit Wkly [Internet]. 2010;55(46):84–91. Available from: https://www.epw.in/journal/2010/46/special-articles/changing-inequalities-utilisation-inpatient-care-rural-india
- O'Donnell P, O'Donovan D, Elmusharaf K. Measuring social exclusion in health-care settings: a scoping review. Int J Equity Health [Internet]. 2018;17(1):1–16. Available from: https://doi.org/10.1186/s12939-018-0732-1
- Peace R. Social exclusion: a concept in need of definition? Soc Policy J N Z. 2011;16:17–35.
- Rafiq M, Yasmeen, Ashfaq, Shalinder, Rifat. Health problems of the elderly in Budgam district (J&K): a cross-sectional study. Int J Contemp Med Res. 2016;3(12):3456–8.
- Strasser R. Rural health around the world: challenges and solutions. Fam Pract [Internet]. 2003 Aug;20(4):457–63 [cited 2025 May 21]. Available from: https://doi.org/10.1093/fampra/cmg422
- The World Bank. Social exclusion and the EU's social inclusion agenda: papers prepared for the EU8 social inclusion study. Washington (DC): The World Bank; 2007.
- Thukral DR. Jammu and Kashmir District Factbook: Ganderbal District. 2nd ed. New Delhi: Datanet India Pvt. Ltd.; 2018.
- Wani RT, Khan S, Dar H. Assessment of facilities available at primary health care centers in Kashmir: a cross-sectional study. Int J Sci Res. 2017;6(6):1–2.
- Wood J. Rural health and healthcare: A North West perspective. Lancaster (UK): Institute for Health Research, Lancaster University; 2004.